“Exhausting drives, thirty or forty patients each day and double visits, overnight stays, and obstetric calls.... And of course, endless sickness; and despite his best efforts, deaths of patients, some of whom were friends or relatives ... deaths sometimes merciful, other times brutal. [He] took no vacations and scarcely missed a day of rounds.... It could not go on. By 1868, in addition to his headaches and, of course, fatigue, he displayed worsening insomnia and periods of agitation.... In the Spring of 1869, shortly after the death of his mother, [his] constitution gave out.” Dr. Owen Wister, an overworked family physician practicing in Germantown, Pennsylvania soon found that he was no longer capable of the effort of so much as writing a prescription. In the words of a non-medical friend describing his condition at the time, “He has neuralgia and nervous weakness from overwork, cannot exert his brain at all, not even to read, and has given up his practice entirely for the present.”
The foregoing paragraph is extracted from the clinical description of Wister’s condition that was presented by the medical historian and internist Steven J. Peitzman in a lecture at the American Association for the History of Medicine in 2007.1 A condition such as Wister’s—in later generations to be known, as Peitzman points out, by the sobriquet “nervous breakdown”—epitomized what would soon be dubbed “neurasthenia.” This latter term first appeared in an article published in The Boston Medical and Surgical Journal (the forerunner of The New England Journal of Medicine) by the eminent nerve specialist Dr. George M. Beard, and was defined as an “exhaustion of the nervous system” and “impoverishment of nerve force, a problem significantly more often encountered in women than in men.” The treatment, providing the patient could afford it, consisted of rest and diversion far from the site of travail, preferably by taking the baths at one of the many spas of America and Europe, or of leisurely travel for an extended period of time. Wister’s slow peregrinations took him first to Saratoga Springs, then to Newport, and thereafter on a grand tour of Europe. When he re-established his practice after three years of this kind of deliberately slow recovery, he chose to do it in a somewhat less demanding location, where he was able to circumscribe his activities and avoid the demands of his former patients. He never again suffered from neurasthenia.
But in 1875, the neurologist S. Weir Mitchell of Philadelphia (who had himself suffered a nervous breakdown nine years earlier) introduced a more directed therapy for the condition, and touted it in fact as a cure.2 Edward Shorter, arguably North America’s leading historian of psychiatry, describes the new treatment as follows in his important—if sometimes exasperating—new book: the patient was put to bed in a private room supervised by the authoritarian doctor and a tough-minded nurse, started on a milk diet, and given intermittent doses of massage and peripheral electricity, often over a period of months. Since the increasingly popular treatment could best be provided in a hospital-type environment, a host of dedicated private clinics soon sprang up all over America and Europe, usually directed by physicians but some owned by entrepreneurial laymen. It is important to note that such physicians were not psychiatrists. The latter treated what was called “mental disease,” namely psychosis, severe depression, and dementia; the former, general physicians, were concerned only with neurasthenia, considered a disease of exhausted nerves.
As described by Shorter, five kinds of symptoms encompassed the range of problems that were identified in nervous exhaustion, neurasthenia (a term that has been little used since the early 1940s), or, as he now proposes to call the loosely defined problem, “nerves.” These were: pathological fatigue going beyond ordinary tiredness; mild depression; mild anxiety; bodily symptoms such as insomnia, chronic pain, and disordered bowels; and some variety of obsessive thinking even though the patient realizes that the ruminations are irrational. He refers to this group of symptoms as constituting a syndrome. This syndrome, he argues, is quite different from major depression, which he prefers to call “melancholia.”
Thus, early in his book, Shorter introduces his readers to two distinct forms (and by implication, two different causes) of what is today collectively known as “depression,” respectively to be called “nerves” and “melancholia.” He proposes that all patients now carrying a diagnosis of depression should be re-categorized into those suffering from one or the other. So different are they, he asserts, that he considers melancholia to be “a predominantly biological illness,” so biologically determined and specific that an adrenal-dependent blood test, the dexamethasone-suppression test (regrettably, he says, now rarely used), will most often be found to be positive in its presence but negative in other psychiatric illnesses. Unlike nerves, a condition symptomatic of the existential tensions with which so many of us live our daily lives, melancholia is “one of the most terrible afflictions in medicine.” It is “fearsome in a far different way than nervousness, for it may lead to despair, hopelessness, a complete lack of pleasure in one’s life, and suicide.” It is as different from nerves, Shorter declares, as tuberculosis is from mumps.
Shorter’s credentials to make such a differentiation are remarkably strong. During the course of devoting his long career to studying the history of psychiatry, he has exhaustively studied that complexly labyrinthine discipline itself, almost as though he were preparing for a career as a clinician or laboratory researcher. A dazzling expertise is apparent in his new book, about drug mechanisms and psychiatric disease in general, not to mention the politics of academic jousting. Shorter may very well be as qualified to make judgments and define categories as is the committee of the American Psychiatric Association that every few years issues yet another iteration of the DSM, the Diagnostic and Statistical Manual of Mental Disorders, though that may be faint praise.
Nosology (from the Greek nosos, meaning “disease,” and logos, referring to “study”) is not a sport for the timid, and certainly not for those so scrupulous about rules and order that they demand consistency in all things. As used in medicine, the word refers to the classification of diseases, for which reason one might suppose that it has some sort of principles of predictability that would make sense to a reasonably well-educated person. Not so. Every hope of successive generations of scholars that order might be constructed from the chaotic mess of medical nomenclature has been frustrated. Even diseases recognized in the same historical period have been given names based on characteristics that have no relation to one another, and thus no common criteria. For one example, the Greeks of the Hippocratic era invented the term “carcinoma” for a tumor with the appearance of a crab (karkinos, “crab,” and oma, “tumor”), and then went on to leave us with another familiar illness described as “consumption,” because it seemed gradually to consume its victims. Beginning around that time, there never have been standardized criteria for the ways in which diseases are named.
In the mid-nineteenth century, attempting to instill some permanent conformity into nosology, Rudolf Virchow, others having discovered that a tubercle-like structure characterized the appearance of consumption, insisted on its being called “tuberculosis.” He is the same sensible German who gave us “thrombosis” (the Greek thrombos means “clot”) for a blood clot lying within an artery or vein. Likewise “leukemia” (from the Greek for “white” and “blood”), because the centrifuged blood of its victims demonstrated an abnormally thick layer of white blood cells above the red. Virchow was determined that all nosology should be based on universal criteria, and for this purpose, he uniformly used the microscopic or visible abnormality that characterized the disease: tubercle, clot, white blood. In this, he was attempting to overcome centuries of practices so inconsistent and even capricious that a sexually transmitted syndrome making its first appearance in 1493 in Italy had been dubbed “syphilis” for the somewhat whimsical reason that an Italian physician named Girolamo Fracastoro wrote an epic poem in 1530, in which a shepherd boy named Syphilus insults one of the gods and is punished by developing a horrible disease.
Of course, Virchow’s efforts were ultimately in vain, as demonstrated by the inconsistency of terminology applied to naming such twentieth-century illnesses as the tick-borne Lyme Disease, named for Lyme, Connecticut, from where the first patients hailed; and Legionnaire’s Disease, originally identified in a group of veterans attending a convention in Philadelphia; and Sjögren’s Syndrome, permanently connected to its discoverer. Obviously no rhyme or reason was applied in pinning a label on any of them. As so often in the past, caprice led the way.
Even if their ways of being named are inconsistent, physicians generally comfort themselves that entities considered to be distinct diseases bear a set of equally distinct and associated physical and laboratory findings. By and large, this is true in internal medicine, but the closer one comes to pathologies of the nervous system the further away is certainty, especially if the illness is one of those we call mental. The first serious attempt to put some order into the confusion was made in 1798 by Philippe Pinel, the chief physician at the Salpêtrière, a Parisian public facility for the insane. In his masterwork, Nosographie philosophique ou méthode de l’analyse appliquée à la médecine, Pinel divided the institutionalized insane into four types, designated as maniacs, melancholics, dementeds, and idiots. There would have been no reason for the hospitalization of those people later to be known as neurasthenics, so Pinel’s experience, coming only from his contact with psychotics and seeming psychotics, was limited to the very sick.3
Even in the next century, it was family physicians who cared for those whose problems were of a nervous sort, as psychiatrists limited themselves to working with the four groups of Pinel. Nowadays, of course, the care of all patients with mental illness is the province of the specialty of psychiatry. Of the many consequences of this development, there has been a strong tendency to lump truly serious disease into the same bundle as conditions of a far less consequential nature. These latter are conditions, Shorter seems to be claiming, that have no biological substrate, or have a connection to physiological phenomena that is rather the result of the problem and not its cause.4
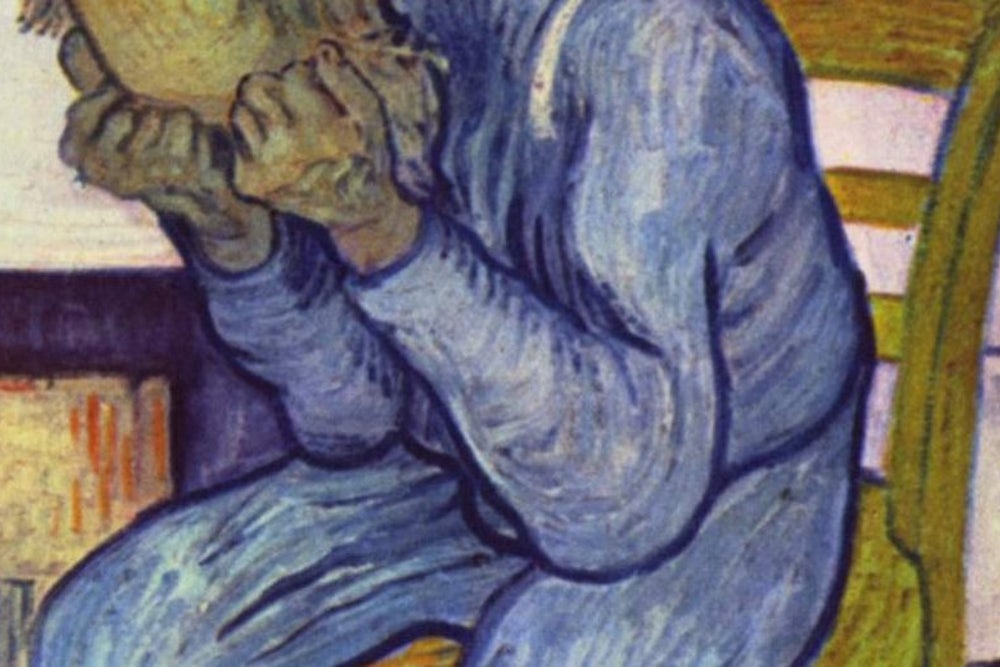
It should not be thought that by choosing to use such a seemingly non-medical word as “melancholia” Shorter is invoking a term more comfortably issuing from the mouth of a layman than that of a highly trained psychiatrist. Melancholia, as a word and as a disease, has in fact enjoyed a long history in medicine, having been introduced during the Classical period and named on the basis of the Greek theory of diseases that most are caused by imbalances of the four humors: blood, phlegm, yellow bile, and black bile, each of which was thought to impart certain personality characteristics. Black (melas) bile (kholē) was believed to instill a dark, depressive cast into one’s outlook, so much so that excessive amounts of it caused the severe depression called “melancholia.” Melancholia was so serious a disease that medieval textbooks of medicine often pictured a typical victim lying in a bed from which he was unable to rise, and being cared for by a woman sitting patiently at his side.
But even during the long period of almost two millennia in which the theory of humors dominated medical thought, the name of this disastrous disease was already being used to refer to much less consequential conditions that later generations would call “nervous weakness” or “neurasthenia.” Well before those two terms came into being, society and the profession of medicine had created a disorder called “Spleen.” It derived its name from the purplish organ where black bile was thought to be both made and destroyed, and whose physiological purpose has puzzled (and continues to puzzle) biologists since the first time human eyes set sight on it. Though we now know a great deal more about the spleen’s usefulness to the body than we did in the historical past, some of those puzzles remain unsolved. Since it was traditionally thought to be the source of melas kholē, all symptoms related to depressed mood and emotional malaise were attributed to it, particularly in seventeenth- and eighteenth-century Britain and somewhat less in contemporary France; many literary works, of which Baudelaire’s unfinished collection of prose poems, Le Spleen de Paris, is perhaps the most famous, attest to its prevalence there.
The symptoms attributed to Spleen varied along a continuum, from the extremes described by Robert Burton in 1621 in The Anatomy of Melancholy to a set of discomfitures so common that the condition became rather fashionable among the upper classes, in time being referred to as the English Malady. The English Malady, in fact, is the title of a medical volume on nervous diseases in general, and those related to Spleen in particular, that was published in 1733 by the leading British physician George Cheyne, who wrote of its distempers, vapours, and lowness of spirits, referring to “these nervous disorders being computed to make almost one third of the Complaints of the People of Condition in England.” Since only “People of Condition” were likely to be seen in Cheyne’s extensive private practice, he seemed not aware of the number of his charity patients who suffered from similar symptoms but would never think to discuss such relatively minor problems with the eminent physician who saw them for major medical conditions such as tuberculosis, cancer, or paralysis.
At the other end of this Splenic continuum was the anguish characteristic of a syndrome that is recognizable as the melancholy that Edward Shorter would have us distinguish from its far lesser associations. These are associations, as we have seen, that existed—Shorter to the contrary—centuries before the often deliberate befuddlement and intermixing caused nowadays by the best and worst intentions of physicians, psychiatrists, the drug industry, and advertising agencies. Here follows Burton’s description, as expressed in the final six lines of a poem of forty-eight couplets that preceded the text of his 740-page book. Every man or woman who has been sufficiently depressed to require hospitalization—as l have—will recognize the anguish expressed by these words:
My pain’s past cure, another hell,
I may not in this torment dwell!
Now desperate, I hate my life,
Lend me a halter [hangman’s noose] or a knife;
All my griefs to this are folly,
Naught so damn’d as melancholy.
And so Shorter seems to be right and he seems to be wrong: persistent moderate instabilities of mood, energy, visceral function, malaise, and similar “nervous exhaustions”—in a word, what he would have us recognize as “nerves”—had for centuries before the present era been lumped together with the much more dangerous diagnosis that we are urged to call “melancholia.” But for those patients suffering from the most debilitating symptomatology, it cannot be doubted that the latter term was more likely to be invoked than the former.
The historic importance of the great German psychiatric theorist and clinician Emil Kraepelin (1856–1926) lies most significantly in his attempts to invoke order amid the chaos that was the classification of mental diseases around the turn of the twentieth century. In 1896, in the fifth edition of his classic work, translated into English as Psychiatry: A Textbook for Students and Physicians, he essentially “killed off melancholia and prompted its replacement with depression,” in Shorter’s account. Though seventeen years later Kraepelin “suggested that particularly malignant outcomes might be referred to as melancholic.... the term melancholia disappeared as an independent disease entity.” Thus with one sweep of the Geheimrat’s nosological authority, an entity that had been recognized since antiquity was driven from the diagnostic arena, an event that occurred at the very beginning of the several-decade period during which leadership in psychiatry was gradually passing from the German-speaking countries to those communicating in English.
This might have been the time for the profession to recognize that its future hopes for a rational nomenclature lay not in the treacherous quicksand of diagnostic categories but rather in the more realistic fields of symptom description and the individualization of therapy. But diagnosis and therapeutics were changing rapidly at the time, as the precision of medical science increasingly became paramount, so that the doctors of the mind no doubt began to feel that their validation lay in classification, order, and predictable nosology, in order to follow the lead of their brethren in internal medicine. They were mistaken then and they are very likely mistaken now. Only the emerging specialty of psychoanalysis seemed to understand that mental maladies are not fully analogous to physical disease. They resist classification, and might better be known by their symptoms and the individualized sufferings of patients than by assigned names.
Once the notion of depression had begun to dominate the diagnostic armamentarium, it became but a matter of time before patients with relatively mild disorders of mood or anxiety would be entered into it. Shorter is particularly good in his meticulous documentation of the ways in which the term came to be used to include—once again as in past centuries, though he does not acknowledge it—the entire range of disturbances, from those that were catastrophic and truly life-threatening to those that he would like us to call nerves. It is in this documentation that his book finds its greatest strength and its greatest weakness: Shorter’s meticulous roll call of pharmacological (in both the scientific and commercial sense) advances will be invaluable to historians and to those seeking to understand how psychiatry and the DSM found themselves in their present diagnostic quagmire, but it will prove maddening to the general reader trying to keep track of all the webwork of influences, well-intentioned and baleful, that have brought us to our present bewilderments.
As the years passed, and as more and more pharmacological treatment methods reached the marketplace—particularly in the relatively recent case of the selective serotonin re-uptake inhibitors (ssris), such as Prozac and its cousins—more and more people were given the diagnosis of depression, increasingly as if there were no difference between the melancholic and the nervous varieties. The leading villains in this ever-widening scenario, as might be expected, were the drug companies and their advertising campaigns, presenting to physicians and the public an ever-greater array of what are called anti-depressants, anxiolytics, tranquilizers, mood stabilizers, and more. But the specialty of psychiatry (and its frustrated attempts at specific nosology, as in the DSM) must bear part of the blame, as also must the practitioners of internal medicine, who diagnose and pharmaceutically treat what they diagnose as depression at the drop of a symptom. This tendency is so widespread that it has entered our cultural perception, and even our television screens, and the demand by patients for drug treatment expands with time. There may even be an element of trendiness in it, and a social association with Cheyne’s “People of Condition.”
“How did everyone become depressed,” asks Shorter, about two-thirds of the way through his book, although he has by that time largely answered his own question. Incorporated into the diagnosis has been every symptom-complex that was in an earlier day lumped into Spleen, from the serious illness recognized since antiquity to the ennui of bored housewives and the chronic neurotic dissatisfaction of those millions who descend into the subway each morning to earn their daily bread. Shorter attributes the contemporary prevalence of diagnoses of depression to the blameworthy commercial actors noted above, but he barely gives reference to the precedent and long life of the notion of Spleen. I would argue with this historical inaccuracy, and propose that a societal tendency toward finding neurotic manifestations in daily life has been an underlying and frequent tendency—at least during certain historical periods—of human nature, to the point where individuals need the reassurance of believing they have a disease with a specific name, when they are only the victims of existential malaise. That modern psychiatry and the pharmaceutical industry have found an intellectual and commercial bounty in this tendency is contributory but hardly the underlying etiology: If my troubles have a name—whether it be depression, Spleen, or whatever—I am sick, and not just neurotic. I need treatment.
Along comes Edward Shorter with a remedy: let us go back to the simplicity of the two very different orders of this particular form of human misery, by calling them respectively “melancholia” and “nerves.” In this day of increasingly complex nosologies and increasingly controversial DSMs, his proposal comes like a cooling blast of fresh air.5 Though I disagree with Shorter about many things—the degree of culpability of the assigned culprits; the totality of influence of modern trends in pharmacology, the pharmaceutical industry, and the psychiatric profession; the statement that “the current crop of drugs referred to as antidepressants are ineffective in real depressive illness, which is to say melancholia, and somehow land wide of the mark in treating nervous illness”; the usefulness in major melancholia of the dexamethasone-suppression test in severe cases; his failure to acknowledge the role of a probable biological element in the condition that he calls “nerves”; and certain denigrations of the validity of psychoanalytic theory—I applaud his contribution, and earnestly believe it should be taken seriously by both the profession and the public, even though the latter must face the implications, social and otherwise, of the reality that one can experience a set of symptoms that amount only to “nerves.”
In certain ways, this is a landmark book. But its overly meticulous and unnecessary inclusion of so many minor details of society’s trudging toward inclusion under the umbrella now indiscriminately called “depression” makes it more difficult to read than it should be. Shorter’s raging torrent of documentation—so helpful to the historian but a hindrance to the general reader and even to most psychiatrists—will necessarily detract from his book’s usefulness as a well-reasoned argument for a straightforward and meaningful differentiation of symptoms that have since ancient times defied easy classification.
Sherwin B. Nuland is clinical professor of surgery at the Yale School of Medicine and the author, most recently, of The Soul of Medicine (Kaplan).
From Peitzman’s Fielding H. Garrison Lecture, presented annually by a distinguished historian of medicine chosen by the officers of the society.
Mitchell, in addition to being an eminent neurologist, was the prolific author of 19 novels, 30 or 40 short stories and 150 poems—all of this in addition to his 35 scientific papers and 3 books. Contemporary critics wrote highly of his literary works.
Pinel is often remembered as the first psychiatrist to remove the chains with which institutionalized patients were often shackled.
- DSM-5 has just appeared. Its editors clearly state that methods of nomenclature are designed to be in accordance with those used in other branches of medicine.
Sir William Gowers, whose two-volume Manual of Diseases of the Nervous System was called “the Bible of neurology” for decades after its publication in 1879, concludes his section on neurasthenia with the following sentence: “It is often better not to gratify the craving for nomenclature that is manifested by many patients, but rather to explain to them that to give their ailments a definite name would involve more error than truth.”