A young, fit U.S. soldier is marching in a Middle Eastern desert, under a blazing summer sun. He’s wearing insulated clothing and lugging more than 100 pounds of gear, and thus sweating profusely as his body attempts to regulate the heat. But it’s 108 degrees out and humid, too much for him bear. The brain is one of the first organs affected by heat, so his judgment becomes impaired; he does not recognize the severity of his situation. Just as his organs begin to fail, he passes out. His internal temperature is in excess of 106 degrees when he dies.
An elderly woman with cardiovascular disease is sitting alone in her Chicago apartment on the second day of a massive heatwave. She has an air conditioner, but she’s on a fixed income and can’t afford to turn it on again—or maybe it broke and she can’t afford to fix it. Either way, she attempts to sleep through the heat again, and her core temperature rises. To cool off, her body’s response is to work the heart harder, pumping more blood to her skin. But the strain on her heart is too much; it triggers cardiac arrest, and she dies.
Such scenarios could surely happen today, if they haven’t already. But as the world warms due to climate change, they’ll become all too common in just a few decades—and that’s according to modest projections.
This is not meant to scare you quite like this month’s cover story in New York magazine, “The Uninhabitable Earth.” That story was both a sensation and quite literally sensational, attracting more than two million readers with its depiction of “where the planet is heading absent aggressive action.” In this future world, humans in many places won’t be able to adapt to rising temperatures. “In the jungles of Costa Rica, where humidity routinely tops 90 percent, simply moving around outside when it’s over 105 degrees Fahrenheit would be lethal. And the effect would be fast: Within a few hours, a human body would be cooked to death from both inside and out,” David Wallace-Wells writes. “[H]eat stress in New York City would exceed that of present-day Bahrain, one of the planet’s hottest spots, and the temperature in Bahrain ‘would induce hyperthermia in even sleeping humans.’”
These scenarios are supported by the science. “For heat waves, our options are now between bad or terrible,” Camilo Mora, a geography professor at University of Hawaii at Manoa, told CNN last month. Mora was the lead author of a recent study, published in the journal Nature, showing that deadly heat days are expected to increase across the world. Around 30 percent of the world’s population today is exposed to so-called “lethal heat” conditions for at least 20 days a year. If we don’t reduce fossil-fuel emissions, the percentage will skyrocket to 74 percent by the year 2100. Put another way, by the end of the century nearly three-quarters of the Earth’s population will face a high risk of dying from heat exposure for more than three weeks every year.
This is the worst-case scenario. Even the study’s best-case scenario—a drastic reduction in greenhouse gases across the world—shows that 48 percent of humanity will be exposed regularly to deadly heat by the year 2100. That’s because even small increases in temperature can have a devastating impact. A study published in Science Advances in June, for instance, found that an increase of less than one degree Fahrenheit in India between 1960 and 2009 increased the probability of mass heat-related deaths by nearly 150 percent.
And make no mistake: Temperatures are rising, in multiple ways. “We’ve got a new normal,” said Howard Frumkin, a professor at the School of Public Health at the University of Washington. “I think all of the studies of trends to date show that we’re having more extreme heat, and we’ve having higher average temperatures. Superimposed on that, we’re seeing more short-term periods of extreme heat. Those are two different trends, and they’re both moving in the wrong direction.” Based on those trends, the U.S. Global Change Research Program predicts “an increase of thousands to tens of thousands of premature heat-related deaths in the summer ... each year as a result of climate change by the end of the century.” And that’s along with the deaths we’ve already seen: In 2015, Scientific American noted that nine out of the ten deadliest heat waves ever have occurred since 2000; together, they’ve killed 128,885 people.
In other words, to understand how global warming wreaks havoc on the human body, we don’t need to be transported to some imagined dystopia. Extreme heat isn’t a doomsday scenario but an existing, deadly phenomenon—and it’s getting worse by the day. The question is whether we’ll act and adapt, thereby saving countless lives.
There are two ways a human body can fail from heat. One is a direct heat stroke. “Your ability to cool yourself down through sweating isn’t infinite,” said Georges Benjamin, executive director of the American Public Health Association. “At some point, your body begins to heat up just like any other object. You go through a variety of problems. You become dehydrated. Your skin dries out. Your various organs begin to shut down. Your kidneys, your liver, your brain. As gross as this may sound, you in effect, cook.” (So maybe Wallace-Wells wasn’t being hyperbolic after all.)
Heat death can also be happen due to a pre-existing condition, the fatal effects of which were triggered by high temperature. “Heat stress provokes huge amounts of cardiovascular strain,” said Matthew Cramer of the Institute of Exercise and Environmental Medicine. “For these people, it’s not necessarily that they’ve cooked, but the strain on their cardiovascular system has led to death.” This is much more common than death by heat stroke, but is harder to quantify since death certificates cite the explicit cause of death—“cardiac arrest,” for instance, rather than “heat-related cardiac arrest.”
In both scenarios, the body’s natural ability to cool itself off through sweating has either reached its capacity or has been compromised through illness, injury, or medication. There are many people who have reduced capacity for sweating, such as those who have suffered severe burns over large parts of their bodies. Cramer, who studies heat impacts on burned people, says 50,000 people suffer severe burn injuries per year in America, and the World Health Organization considers burns “a global public health problem,” with the majority of severe burn cases occurring in low- and middle-income countries.
Bodies that are battling illness or on medication may also struggle with heat regulation. Diuretics tend to dehydrate people; anticholinergics and antipsychotics reduce sweating and inhibit heat dissipation. An analysis of the 2003 heat wave in France that killed 15,000 people suggested that many of these deaths could have been avoided had people been made aware of the side effects of their drugs. As for illnesses, “Anything that impairs the respiratory or circulatory system will increase risk,” said Mike McGheehin, who spent 33 years as an environmental epidemiologist at the Centers for Disease Control and Prevention. “Obesity, diabetes, COPD, heart disease, and renal disease.” Kidney disease, mental illness, and multiple sclerosis. The list goes on and on.
This summer has presented many opportunities for bodies to break down from heat. Temperature records, some more than a century old, have been broken across California, Nevada, Utah, Idaho and Arizona. (Speaking of Arizona, it’s been so hot there that planes can’t fly.) And it’s not just America. Last month, Iran nearly set the world record for highest temperature ever recorded. The May heatwave that hit India and Pakistan set new world records as well, including what the New York Times called “potentially the hottest temperature ever recorded in Asia”: 129.2 degrees Fahrenheit. Worldwide, 2017 is widely expected to be the second-hottest year, after 2016, since we began keeping global average temperature records in 1880.

These trends have public health professionals concerned about how people are going to deal with the heat when it comes their way. “Clearly this is one of the most important problems we’re going to see from a public health perspective,” Benjamin said. “This is not a tomorrow problem. It’s a significant public health problem that we need to address today.”
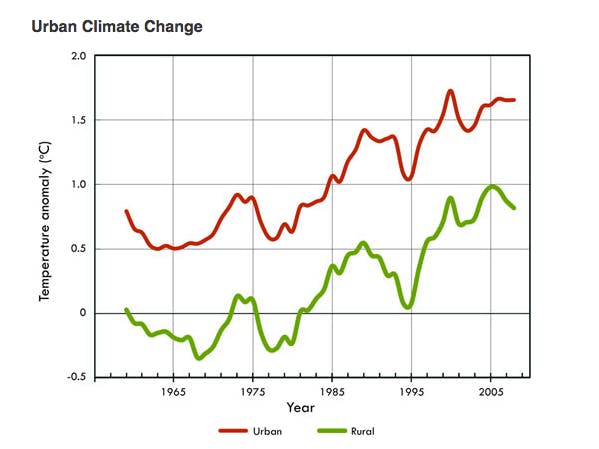
It’s a public health problem especially in cities, says Brian Stone, a professor at Georgia Tech’s City and Regional Planning Program. “Our fundamental work shows that larger cities are warming at twice the rate of the planet,” he said, describing a phenomenon known as urban heat islands, where built-up areas tend to be hotter than surrounding rural areas, mainly because plants have been replaced by heat-absorbing concrete. Global warming is making that phenomenon worse. “We’re really worried about the rate of how quickly we’re starting to see cities heat up,” Stone said.
According to Stone’s analysis, the most rapidly warming city is Louisville, Kentucky, followed by Phoenix, Arizona, and Atlanta, Georgia. But he’s less concerned about cities like Phoenix, which already have infrastructure to deal with brutally high temperatures, than he is about Chicago, Buffalo, and other cities in the northern United States that have really never had to deal with extreme heat. That is precisely why the Chicago heat wave of 1995 that killed 759 people was so deadly. According to the Chicago Tribune, the city was “caught off guard,” and had “a power grid that couldn’t meet demand and a lack of awareness on the perils of brutal heat.”
In other words, Stone and others say, excessive death rates are not always due to just extreme temperatures, but unusual temperatures. People are more likely to die when they are confronted with temperatures they don’t expect and thus aren’t prepared for. That’s why officials in cities not experiencing heat-related extremes need to improve emergency response systems, now. “Those people have got to start thinking in term of, ‘two years ago we had four hot days, the year after we had eight hot days,’” Benjamin said. “Public health systems should be put in place to respond to prolonged heat waves. Emergency cooling centers where people can go should be built. Identify where the people who are most socially isolated live.” Absent preventative action, heat-related deaths in New York City could quintuple by the year 2080, according to recent research.
Some cities have already started to prepare. Stone recently completed a heat adaptation study for Louisville that includes not only emergency management planning but also ways the city can prevent itself from getting so hot (by improving energy efficiency and installing green roofs, for instance). But as for now, he said, it’s rare to see a city actually adopt policies supportive of heat management. “We do see flooding adaptation plans—New York City has one, and New Orleans has one—but heat adaptation planning is a very new idea, in the U.S. and really around the world,” he said. “It takes a lot to convince a mayor that a city can actually cool itself down. It’s not intuitive.”
The good news is that humans adapt to heat, both physiologically (through acclimatization) and socially (with air conditioning, for instance). That will continue, according to the U.S. Global Change Research Program, which states with very high confidence that adaptation efforts in humans “will reduce the projected increase in deaths from heat.”
But there’s a limit to this. “There’s no way to adapt to heat that’s more than a certain amount,” Frumkin said. “And socially, there’s always going to be people we miss, who don’t have access to air conditioning.” McGeehin noted those people will likely be poor, elderly, and minority populations. “It’s a quintessential public health problem in that it impacts the most disenfranchised of our society. Young, healthy, middle-class people will largely be left alone,” he said.
Air conditioners also have limits, especially in cities where blackouts can occur. “It is inevitable,” Stone said, that large cities will see blackouts during future heat waves. “The number of blackouts we see year over year is increasing dramatically,” he said. “Whether that’s caused by the heatwave or just happens during the heatwave doesn’t really matter.... The likelihood of an extensive blackout during a heatwave is high, and getting higher as we add more devices and stressors to the grid.”
It’s a “cruel irony,” Frumkin said, that as the world gets hotter, we need more air conditioning, and thus consume more electricity. And if that electricity comes from fossil fuel sources, it will create more global warming, which in turn will increase the demand for air conditioning. The answer, he said, is to “decarbonize the electric grid.” But that’s easier said than done, especially when the Trump administration is devoted to increasing the use of fossil fuels to support the country’s electrical grid.
As with many other efforts to fight climate change, though, cities don’t need Washington’s help to take action on heat adaptation. “Cities can manage their own heat islands on their own, and that’s where we most need to be focused,” Stone said. But that will require convincing elected leaders that extreme heat is big a threat as, say, rising seas—and one that can’t be addressed with something as obvious as a sea wall. That’s the challenge, says McGeehin: “Heat as a major natural disaster is mostly overlooked in this country.” It’s a quiet killer, and perhaps more lethal because of it.
Correction: Howard Frumkin is no longer the dean of the School of Public Health at the University of Washington. He’s a professor.
