Humans and pigs share 98 percent of the same genes. Most of those similarities don’t matter—we share genes with a lot of animals. But a small number of specific similarities do: They make it possible to use porcine tissue for human ends. And with recent developments in gene editing technology, knocking down a few pesky genes that would otherwise cause the human immune system to reject foreign organs allows for the use of entire pig organs in human patients. This process is called xenotransplantation, and on January 7 it saw a breakthrough when a team at the University of Maryland Medical Center in Baltimore successfully completed the first ever transplant of a genetically modified pig’s heart into a terminally ill human patient.
Celebration of this momentous occasion was quickly eclipsed by ethical debate about the procedure. The medical team rushed the risky transplant as an emergency surgery, and the patient, David Bennett Sr., was a convicted violent criminal, chosen over other potential patients. But as bioethicists rushed to defend this particular procedure, and the need for xenotransplantation more broadly, they were mum on the ethics of creating a new category of animal farming: a standing reserve of genetically modified animals bred as repositories of organs for human use. Transfixed by the promise of a world where patients no longer die waiting for their transplant number to come up, many seem to have overlooked an important caveat: We are still very far from being able to divorce transplants from the question of who deserves moral consideration, and why.
Modern bioethics rests on four basic principles to determine whether a procedure is ethical: autonomy, justice, beneficence, and nonmaleficence. In short, this means that a medical procedure is considered to be ethical if the patient agrees to it of their own free will, they do not receive preferential treatment, and the procedure is conducted in good faith, meaning that doctors intend to help rather than harm their patient.
Bennett’s pig heart raised ethical eyebrows because the procedure is highly risky—the longest-surviving previous recipient of a pig heart was a baboon who survived less than two months with the transplant. Then there was Bennett himself. In 1988, he repeatedly stabbed Edward Shumaker at a bar in Hagerstown, Maryland, leaving him paralyzed from the waist down. Shumaker would survive 19 more years in ill health before dying in 2005. Bennett served six years of a 10-year sentence on weapons and battery charges and did not pay any of the $3.4 million in damages he was ordered to pay Shumaker’s family. When this fact was reported after the surgery had already been completed, critics—including Shumaker’s family—wondered why someone more deserving hadn’t been chosen for another chance at life.
From a bioethics perspective, however, neither of these are problems. A cornerstone of medical justice is that it differentiates itself from criminal justice: A heart transplant for a criminal or convict is the textbook case for why medical care should not morally discriminate between people in need of care based on their past actions. And since Bennett agreed to the surgery and the doctors did their best to ensure he survived (he is still alive at the time of this writing), the four principles hold—even though Bennett’s one-year survival chances are probably significantly below the roughly 85 percent average for traditional heart transplant patients.
Regardless of what happens to Bennett, the transplant may be a watershed moment for a branch of medicine long plagued by supply issues. At any given moment, well over 100,000 people in the United States with severe organ disease languish on waiting lists for transplants. Those transplants require either living donors (kidney and liver donations can come from a live donor) or more likely dead donors (for hearts). Demand usually outstrips supply, and 17 people on average die every day waiting for organs that don’t arrive on time. This makes the prospect of a reliable and renewable source of organs appealing. The most renowned bioethicists in the country have gone so far as to claim, “There is no question that using pigs as organ sources is the future.”
There’s just one hitch: the pigs themselves. Assuming that pigs are the future of xenotransplantation assumes that there is no ethical problem with creating a new form of animal farming predicated on genetic modification and on-demand slaughter for spare parts. And yet a surprising number of medical professionals, bioethicisists, and the media covering xenotransplantation have been mum on the subject. This attitude is best encapsulated by a comment the pathbreaking bioethicist Arthur Caplan made in an interview with The New York Times, while defending Bennett’s right to the surgery. “To be clear, he didn’t take a human organ from anybody,” Caplan told the Times. “Nobody died because this guy got a pig heart.”
Xenotransplantation hinges on this foundational but silent assumption: that the lives of the animals used to produce organs do not matter, or at least that they matter much less than the human lives they might save. Scientific progress has long relied on the same assumption.
Animal testing and the use of animal models has been foundational to the development of much of modern medicine. While we may have progressed since René Descartes claimed in the seventeenth century that animals were automata incapable of feeling pain (and vivisected dogs without anaesthesia to prove the point), society is more committed than ever to building our medical progress on a foundation of animal corpses. Animal testing is extremely secretive, and few institutions and countries keep or allow access to records, but the best estimate places the number of animals sacrificed on the altar of science at 200 million per year globally, including over 14 million in the U.S.
The commercial use of animal parts for medical purposes is an equally flourishing business. Due to their similarity to humans, pig heart valves are repurposed for human heart valve replacements and pig tissues are used for the manufacture of pharmaceuticals like the anticoagulant heparin (until the early 2000s, some insulin was still produced from pigs’ pancreases). The business is large enough that pork giant Smithfield Foods even has a dedicated bioscience branch.
Ethically speaking, the use of animals for medical purposes is thorny. While eating animals prioritizes humans’ gustatory pleasure (your love for bacon) above animals’ interest in not experiencing pain or being killed, leading many ethicists to consider it unethical except in particular contexts, the medical question changes the stakes, weighing the life and suffering of both currently existing and future humans against the life and suffering of animals. If a medicine can save many humans, is it not worth killing some lab mice or beagles to get there? If pigs’ hearts can save people dying on organ waiting lists, is it not worth killing some pigs and baboons?
This is the position that the medical establishment and university Institutional Animal Care and Use Committees, or IACUCs, which review animal research, take explicitly. As far as bioethics considers animals, it tends to focus on the so-called 3 R’s (replace, reduce, and refine the use of animals), a much lower ethical standard than that applied to human research subjects, and one enforced far less rigorously. This is also the position that many laypeople take implicitly. Most of us don’t like to think about a pig being killed and having her heart cut out and implanted into the body of a previously healthy baboon, whose heart was also cut out, and then that baboon dying a few weeks later—all for the sake of peer-reviewed publications. But on principle we accept the desirability of medical advances that will potentially save human lives. This is anthropocentrism—the view that humans have moral primacy above all other beings—and because we are human, it comes naturally to us.
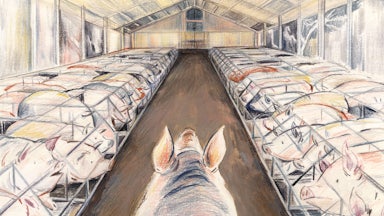
The problem with a pig organ transplant, however, is that it doesn’t rely on a simple ethical decision of whether any given pig’s life is worth less than that of any given human who needs a heart. Rather, it calls for the creation of a new type of farming and a new political economy of animal use.
The heart transplanted into Bennett was provided by a Virginia company called United Therapeutics, which is in the process of patenting its proprietary xenoheart, to be grown inside a population of pigs genetically modified specifically to create human-compatible organs. The issue here is less that a corporation is genetically engineering animals and patenting a new technology (although of course that matters) but rather that embracing xenotransplantation involves embracing the commodification, modification, and slaughter of animals on an unknown scale. This makes it a systemic question about the role of animals in our society.
Usually when the medical ethics of animal use are discussed, the question is posed like this: If it’s a human or a pig, if it’s you or a pig, which do you choose? But reality is not a philosophical thought experiment, an isolated moral decision about the fate and worth of individuals in unique circumstances.
In reality, creating the situation where a pig heart can be transplanted into that of a human takes years of biomedical research, peer-reviewed publications, medical teams sacrificing pigs and baboons to science, and a company that breeds these specific genetically modified pigs and hopes to make them a mass-market product. None of this happens in isolation. And none of these trade one animal life for one human life; multiple animals have to be killed for every human potentially saved. There are value systems and value chains building off each other, preparing to sacrifice pigs profitably and systemically in the interest of human health. That’s a different scale of ethical problem, and while it might not change the ethical calculus for many, it just might make the ethical question more complicated than Caplan suggested when he dismissed the pig slaughtered for Bennett’s heart as “nobody.”
In the wake of Bennett’s surgery, there will now be many questions, including about the ethics of genetic modification of animals and of future human clinical trials, about regulatory and policy frameworks for xenotransplantation, and about who gets these still experimental heart transplants. But there is one that should not be ignored: How can we work toward a medical system that doesn’t have to rely on the suffering and death of animals so that humans can thrive? There is already a robust activist and research community pushing for alternatives to animal models in scientific and medical research, and the 3-D printing of synthetic organs has shown promise, with a successful transplant in Boston in 2018 of a bladder grown from the patient’s own cells. Research on 3-D-printed human hearts as both medical models and potential transplants is also underway. Pursuing this research not only has broader medical applications but is far more desirable from an ethical perspective.
Many, including many bioethicists, will shrug off this concern for animals as maudlin or perhaps even misanthropic, but if we take the bio in bioethics to mean concern with all of life and not simply human life, then the question of animal ethics becomes central to the morality of the entire enterprise. It should make us question our assumed supremacy over animals and seek alternatives that allow both humans and nonhumans to thrive.