Last month, cases of flu reached their highest levels in the United States in 25 years. Many hospitals were unprepared for the surge; as emergency wards filled with flu patients, health care workers were left to weather the impacts. As of February 6, there have been at least 22 million reported cases, 280,000 hospitalizations, and 12,000 deaths from flu so far this season, according to the Centers for Disease Control and Prevention. Many of those afflicted are being hospitalized due to severe postviral complications, such as pneumonia, antibiotic-resistant staph, and even fatal brain swelling.
And while rates have since subsided, we’re not out of the woods yet, with flu B now on the rise. As epidemiologist Marisa Donnelly said, “We’re still in the thick of the season.”
What explains why recent flu seasons have been so severe? There are several factors.
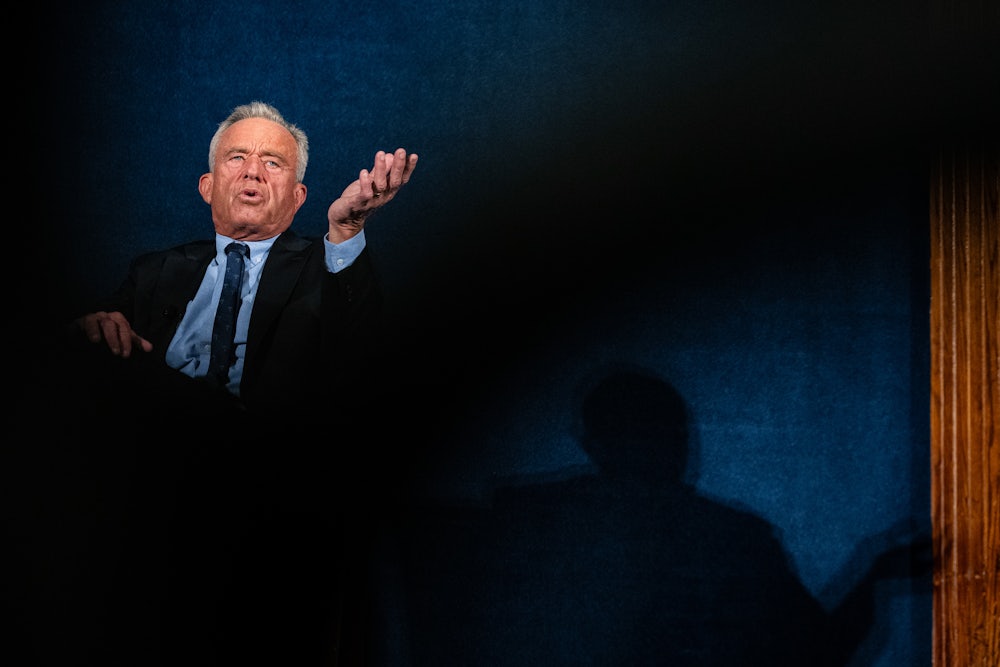
In this political climate, the first thing that may come to mind is the anti-vaccine policy coming from Robert F. Kennedy Jr.’s Department of Health and Human Services, which has sown confusion around vaccines, leading to lower rates of vaccination for the flu and other diseases—not to mention massive preventable measles outbreaks. But it’s also true that the dominant strain of flu may not be well matched to the existing vaccine.
However, a less discussed aspect behind the high rates of flu and disease severity is a slew of recent research finding that prior Covid-19 infections can damage immune responses—and most Americans have been infected with Covid at least once by now.
“It is clear that at least some of what we’re seeing right now is likely related to that immunity problem from Covid-19 infections,” Dr. Ziyad Al-Aly, a clinical epidemiologist at Washington University in St. Louis, and co-author of a study on the subject, told The New Republic.
He’s not the only doctor to connect these dots. According to Dr. Monica Verduzco-Gutierrez, chair of the Department of Rehabilitation Medicine at the University of Texas, El Paso, “Prior Covid-19 infection can lead to persistent immune dysfunction, which may increase susceptibility to subsequent influenza infection and severity of disease.”
Despite this, there is a “pervasive nonchalance” about the surge in flu and spread of other respiratory viruses like Covid among the public, as Al-Aly put it—and RFK Jr.’s moves at HHS are in part to blame, he said. On top of that, hospitals are refusing to adequately staff their wards or protect health care workers from infection, increasing the burden of disease and putting the public at risk. And this week, the FDA decided not to consider Moderna’s application for a new mRNA-based flu vaccine—a decision handed down by the agency’s notorious anti-vaxxer Vinay Prasad.
Overall, under Kennedy’s watch, there has been more chaos, more confusion, and less vaccination—and the consequences have been deadly.
Sixty children have died from the flu this season—the vast majority of whom were unvaccinated—according to the CDC.
In the midst of this unfolding tragedy, the Department of Health and Human Services made the controversial, unilateral decision to slash the childhood vaccine schedule from 17 universally recommended vaccines down to 11. Six vaccines—rotavirus, Covid-19, influenza, meningococcal disease, hepatitis A, and hepatitis B—have been demoted to the status of “shared clinical decision-making.” This status is typically reserved for “situations of genuine clinical equipoise,” wrote Dr. Jake Scott for the Center for Infectious Disease Research and Policy, which does not apply to the six removed vaccines, given the scientific consensus on their safety and efficacy.
HHS was quick to justify its decision, in a paper penned by notorious anti-vax HHS leadership, which went to great lengths to play up the small risks of those vaccines. Its authors wrote that they were aligning vaccine policy with that of “peer” countries like Denmark, when in fact Denmark itself is an outlier among most European countries, according to KFF. It also isn’t a fair comparison: Denmark has a much smaller population and universal health care coverage, meaning many fewer patients fall between the cracks in terms of needed preventative care.
The result of this change will be that fewer parents will come to view the flu vaccine as safe and necessary for their children, experts say.
“Many parents are already unsure if their child needs a flu vaccine, and the secretary’s statements can tip the balance and lead to less use,” said Dorit Reiss, a law professor and vaccine policy expert at the University of California Law, in a statement to The New Republic. “Less vaccines will likely lead to more deaths—among children and adults.” She pointed out that “for influenza, children are a real source of infection for other family members, including the elderly.”
Vaccination rates for children for flu have dropped from 58 to 45 percent since the 2019–2020 season, as of late January, according to the CDC.
“With fewer people vaccinated, you’re seeing the risk of having a severe reaction increase. So that’s definitely a major factor in seeing high flu hospitalizations,” said Donnelly, who also writes the New York edition of the public health newsletter Your Local Epidemiologist.
HHS changing the vaccine schedule followed a year of other unprecedented moves to circumvent and challenge established vaccine policy. The list of changes is dizzying: including HHS’s replacing the members of its vaccine advisory board with vaccine skeptics, cutting access to Covid vaccines, and slashing funding for mRNA vaccine research. This has led to pharmaceutical companies themselves turning away from this important vaccine technology, making note of the anti-vaccine tone set by the government. This comes atop decimating cuts to the CDC.
Meanwhile, many states and major medical associations have maintained their previous vaccine recommendations, citing the changes as not based in science, with initiatives like the Vaccine Integrity Project attempting to fill in the gaps left by the corrupted CDC.
However, patients are “confused” about what they should do given the mixed messaging they are receiving, explained Donnelly. Despite the claims of the Make America Healthy Again movement that they are restoring trust in public health, they are doing the opposite. According to a survey by KFF, less than half of respondents said that they trusted the CDC, the lowest number since before the pandemic.
Inconsistent public health messaging “undermines trust,” said Al-Aly. “All of that political turmoil and misinformation … has a true effect on people’s lives.”
We are already seeing those impacts with measles, he added. “It’s really, really tragic.”
As threats have grown to the public, health care workers on the front lines have found themselves at greater risk, as well. The flu surge has exacerbated overcrowding and understaffing issues for hospital workers in many cases, according to Jane Thomason, the assistant director for Health and Safety at National Nurses United. She said that hospitals didn’t prepare adequately for the flu season despite it being “predictable.”
As she put it, “Employers are just refusing to staff units with the number of nurses needed to care for patients. And then we’re adding in this surge of patients on top of that. And so the impacts here can be really severe, for both patients and nurses.”
In coming years, hospitals will only find themselves further strapped for personnel as the government cuts Medicaid and Medicare and the Affordable Care Act, leaving millions more uninsured. The impact will disproportionately affect low-income hospitals where more patients are on Medicaid. With lower insured rates, more people will delay medical care until it is an emergency and the hospital is their only option. This is especially true for immigrants, many of whom are now terrified to seek medical care as Medicaid shares data with immigration enforcement officers who now lurk around hospitals.
Thomason pointed to the dangers of hospital overcrowding—longer wait times can lead to more deaths and complications. Understaffing can also contribute to staff injuries and workplace violence, according to research published by National Nurses United. In fact, hospitals consistently rank among the most dangerous worksites for employees. These are among the reasons behind the massive New York City nurses’ strike, and they are far from the only nurses protesting for better conditions.
“We’re not just talking about theoretical impacts, or discomfort,” Thomason said. “We’re talking about people dying.”
Cuts to funding for disease surveillance, such as wastewater data, will also leave us less prepared to face the next pandemic, according to Donnelly, who is also the head epidemiologist at Biobot Analytics, a top wastewater research company.
“There was so much invested in building wastewater surveillance infrastructure during the pandemic. And communities really used this as a tool to understand what was going on locally, communicate with the public, inform the public,” she said. “If that funding is taken away, it moves us backwards in terms of preparedness for the next public health emergency.”
Thomason also said that hospitals aren’t doing enough to protect their staff from catching the same respiratory viruses their patients are battling. Often, hospitals don’t provide adequate personal protective equipment to staff, screen patients for respiratory illnesses, employ correct isolation procedures among patients, or prioritize air filtration, she said—all in addition to offering inadequate “nonpunitive” sick leave. “Those are the conditions that are putting nurses at risk of getting an infection at work,” she said, citing a 2024 National Nurses United survey.
Donnelly, Thomason, and Al-Aly all stressed the importance of ensuring widespread vaccination, investing in proper ventilation in health care and other crowded public settings, and using PPE as ways to mitigate surges like these.
“You go to the E.R., and there’s no isolation procedures—people are sitting in a packed E.R. coughing, no mask, nothing, and then literally spreading it around,” Al-Aly said. “And that is a major failure of the hospital system.”