While the Supreme Court decision overturning Roe v. Wade focused specifically on ending the federal right to obtain an abortion, it may have wide-ranging consequences for access to other forms of reproductive health care, including very common, lifesaving procedures for pregnant patients who might never consider having an elective abortion.
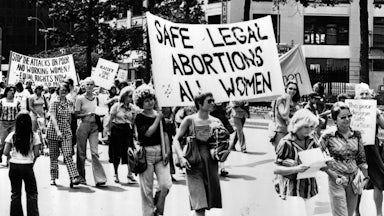
Thirteen states enacted so-called “trigger” laws to ban most abortions immediately or shortly after Roe’s invalidation, and the Guttmacher Institute, which supports abortion rights, estimates that 26 states in total are certain or likely to outlaw abortion in the near term, creating a ragged patchwork of laws dictating reproductive health care across the country. According to analysis by The New York Times, a quarter of women of reproductive age could have to travel upward of 200 miles to obtain a legal abortion—a functional impossibility for those women who may not be able to get time off from work, find transportation for such long-distance travel, or obtain care for any children at home.
The ripple effects of such bans also extend to how medical emergencies may be treated. Abortion bans could complicate care for the 26 percent of pregnancies that end in miscarriages, already an emotionally and physically traumatic experience for the mother. A physician, faced with uncertainty as to whether they’re legally allowed to offer certain forms of care, may be hesitant to treat a person who suffers an incomplete miscarriage, for example, due to concerns that they could be held criminally liable for extracting remaining fetal tissue.
“Clinicians may be thinking that they have to wait, they may be needing to get additional opinions, whether it’s a legal opinion, whether it’s another medical opinion,” said Iffath Abbasi Hoskins, the president of the American College of Obstetricians and Gynecologists, in a press briefing on Friday. “It’s going to have a devastating effect on every aspect of a woman’s health care, including if she is spontaneously miscarrying, but the situation has not completed itself yet.” (An American tourist in Malta who experienced an incomplete miscarriage and was at risk of a life-threatening infection had to be flown to Spain last week to terminate the pregnancy; Malta does not permit abortions under any circumstance.)
Selina Sandoval, an ob-gyn in California and a fellow with Physicians for Reproductive Health, told me that physicians use the same medication regimen for early pregnancy loss as they do for medication abortions in the first trimester. (Dilation and curettage procedures, or D&Cs, are also used for both abortions and for miscarriages to clear tissue from the uterus.)
“We have already—before the Supreme Court decision—seen patients turned away by other providers, by pharmacists, by emergency room physicians, for example, because those people don’t feel that they can confirm what the medications are being used for,” Sandoval said. “So these patients essentially have decreased access to care, [and] they’re going to have worsened health outcomes. These are all things that we knew were coming.”
Given the overlap between abortion care and miscarriage treatment, abortion bans could also affect how physicians are trained. “An important predictor of a physician’s ability to provide a full range of miscarriage management options is having had abortion care training as a resident,” said Rebecca Reingold, associate director for the O’Neill Institute for National and Global Health Law at Georgetown University. “We’re going to see fewer providers receiving the training they need to provide these types of health services. And a shrinking workforce, not only for abortion services but also for the treatment of miscarriages, will have far-reaching consequences for maternal health.”
Confusion about what is and isn’t permitted under an abortion ban could also affect treatment for ectopic pregnancies, which occur when a fertilized egg implants outside the uterus. These pregnancies are never viable, and delays in treatment can result in death. Treatment for these pregnancies is different from abortion care, but physicians and pharmacists may have doubts about what they are legally allowed to provide; already in Texas a woman was denied treatment for her ectopic pregnancy due to confusion over what was permissible under Texas’s stringent abortion law.
Six states prohibit abortions when the fetus may have a genetic anomaly, according to the Guttmacher Institute, and three require counseling on perinatal hospice services before a patient can undergo an abortion based on a lethal condition. Sandoval said that it could be traumatic and dangerous for women to carry a pregnancy to term knowing that their baby would not survive. “We’re forcing these people to continue their pregnancies that will never result in a live birth and undergo deliveries far beyond where they needed to be, when they could have had access to a safe and simple medical procedure,” Sandoval said.
Even the most restrictive abortion laws in the country have exceptions for protecting the health or the life of the mother. (Exceptions focused on the “life” of the mother rather than “health” provide an even narrower scope for circumstances when abortion is permitted.) But these clauses are vaguely defined, often leaving it up to the physician to determine at what point a woman’s life is in danger. This complicates the situation for conditions that are not yet dangerous but will become so as the pregnancy progresses. Some states further require a second physician to approve the termination of a pregnancy to save the life of the mother after a certain point in the pregnancy.
If a doctor is waiting longer than they might otherwise to make a determination about whether the mother’s life is in danger, that exposes her to even greater risk. Jonas Swartz, an assistant professor in the Department of Obstetrics and Gynecology at Duke University, highlighted this uncertainty in a press briefing on Monday: “What degree of medical risk is enough that you decide it’s a medical emergency? Is it a 1 percent risk of death? Is it a 30 percent risk of death? Is it a 50 percent risk of death? Do you have to wait for someone to be actively dying?”
Even if a doctor decides to wait until the last possible moment to administer care, there is still a risk of failure, said Beverly Gray, another associate professor in the Department of Obstetrics and Gynecology at Duke University. “You’re not guaranteed that you’re going to save a life when you wait until a patient is at the brink of death,” Gray said.
The United States already has the highest maternal mortality rate among developed countries, and the rate increased significantly in 2020. One 2021 study found that maternal mortality would increase under a hypothetical abortion ban and reinforce existing disparities: The study found that Black mothers, who already experience disproportionately high maternal mortality rates, would experience a 33 percent increase in deaths in subsequent years after a ban was enacted.
According to Pew Research, based on data from the District of Columbia and 47 states that reported data to the Centers for Disease Control and Prevention in 2019, the majority of women who obtained abortions were in their twenties, and 85 percent were unmarried. In D.C. and the 29 states that provided racial and ethnic data to the CDC, 38 percent of women who obtained abortions were Black, compared to 33 percent who were white and 21 percent who were Hispanic. Seventy-five percent of women who obtained abortions in 2014 were poor or low-income, according to the Guttmacher Institute.
The Supreme Court’s ruling on Roe will reinforce preexisting health disparities, Reingold argued. “We know that abortion bans are going to disproportionately affect women who are already underserved and marginalized: women who are living in poverty or in rural areas, or women of color, or young or undocumented or [who] experienced intimate partner violence,” Reingold said. “Maternal health, maternal morbidity and mortality will only be exacerbated by these types of bans.”