Last week, at an event held by the U.S. Chamber of Commerce Foundation, White House Covid-19 response coordinator Dr. Ashish Jha said that the Biden administration would begin shifting procurement of coronavirus tests and treatments from the federal government to the commercial sector. “One of the things we’ve spent a lot of time thinking about in the last many months … is getting us out of that acute emergency phase where the U.S. government is buying the vaccines, buying the treatments, buying the diagnostic tests,” Jha said, adding that by 2023, “you’re going to see the commercialization of almost all of these products.”
This coming commercialization is but the latest sign that American health care, after glimpses of something better during the pandemic, is returning to business as usual—that is, back to its usual dysfunctional, wasteful, and unequal state.
So much was wrong with America’s response to Covid-19 that it can be easy to forget what was right, including notable departures from usual operating procedures in American health care financing. Covid-related care was usually covered for the uninsured, at least until the program ran out of funds and became defunct in March. Insurers waived co-pays and deductibles for Covid-related hospitalizations—for a time, anyway; average out-of-pocket payments for a coronavirus hospitalization are now around $4,000 for the privately insured. The Families First Coronavirus Response Act, the emergency package that President Trump signed into law in mid-March 2020, helped prevent states from pushing people out of Medicaid, a lifeline that will be cut once the Federal Public Health Emergency is lifted (and an estimated five million to 14 million people lose Medicaid coverage). Finally, the federal government directly procured and provided billions of dollars of Covid tests, treatments, and vaccinations—an approach that will end with “commercialization.”
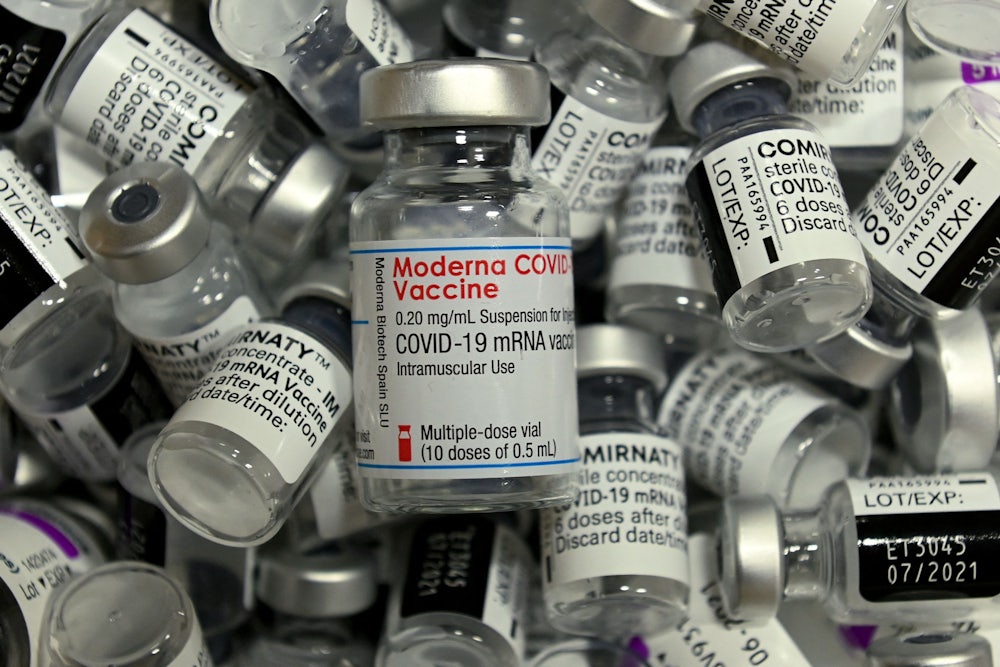
Of course, the vaccines have always been “commercial”: They are manufactured and sold by companies like Pfizer and Moderna. During the pandemic, however, the United States wisely did not relegate procurement of these products to the diverse slew of public and private insurance programs that cover most Americans. Instead, the federal government spent tens of billions on vaccine R&D, while also subsidizing drug firms’ manufacturing capacity and market risk, and it directly negotiated with companies and purchased these life-saving products so it could provide them to the public for free. This had important benefits in terms of the rapid delivery of the vaccines, their cost to society, and their provision in a relatively equitable fashion (within the U.S. only, alas). But as Covid-related care becomes like all else in American health care, those benefits will vanish.
For instance, it’s a truism that Americans get ripped off by drug companies: A 2021 RAND Corporation study found that U.S. drug prices were more than double those in other nations. But the price differentials for Covid-19 vaccines were generally much smaller. According to a Washington Post analysis, relative to the U.S., the European Union paid 24 percent less for the Pfizer vaccine and 15 percent less for Johnson & Johnson but 20 percent more for Moderna. Once they are no longer negotiating with the U.S. government but instead with our jumble of for-profit private insurers, pharmacy benefit managers, state Medicaid programs, and Medicare Part D drug plans, pharmaceutical companies will jack up prices. Moderna CEO Stéphane Bancel said as much in an interview with Yahoo Finance: “So what we are doing as a company is to get ready for a private market situation,” he said, adding that the U.S. price of his firm’s vaccine in the “public setting” was, in his opinion, quite low and that he expects to increase it in “an endemic setting.” Pfizer’s CEO has also alluded to increasing vaccine prices.
We didn’t necessarily get great deals from these firms, however. The American public is—or should be—an owner of the Moderna vaccine: Taxpayers financed its development, and NIH scientists played a key role in inventing it. Also, it’s not as if these companies didn’t turn a hefty profit from their sales to governments: Pfizer and Moderna have taken in $79 billion in revenue for Covid-19 pharmaceuticals globally. To now hand the keys over to a hodgepodge of insurance intermediaries will drive up costs, which will be borne by the public. In addition to increasing health insurance premiums, this could have the effect of squeezing state Medicaid budgets and consequently the availability of funds for other care.
But this is not only about money. We should care about the shift Jha announced because achieving universal and equitable access to Covid-related care remains critical. So far, the government has not only provided the vaccine for free but forbidden providers from charging administrative fees or discriminating based on a patient’s immigration status. Covid therapeutics like monoclonals and oral antivirals (such as Paxlovid) have also been distributed free of charge. Some municipalities took innovative strategies to improve uptake of these agents, ranging from mobile vaccine outreach teams to free home delivery of Paxlovid in New York City—programs that would have been far more costly if health departments also had to buy the products. Yes, disparities in vaccine uptake nevertheless persisted, and inadequate access to health care has remained a barrier to Covid care. In one study, for instance, my colleagues and I found that the uninsured were much less likely to have a booster shot, perhaps because of lack of a trusting relationship with a primary care physician who could provide information and counsel (and the booster itself). That’s not a surprise: Single-disease-focused “vertical” programs are no substitute for comprehensive, universal, primary care–based systems. Still, it’s hard to imagine that the commercialization of Covid care won’t lead to a worsening of disparities.
It’s still unclear how the process of commercialization will unfold and whether steps will be taken to retain some access for the uninsured: The administration is meeting with pharmacists, drug firms, and health departments later this month to work out details. Additionally, under the Affordable Care Act, most insurers are required to cover certain forms of preventive care—including recommended vaccines—for free. In all likelihood, however, bringing these products into the fold of regular American health care will reduce access. Some Medicaid patients could see co-pays for Covid vaccines once they are commercialized—or not have access to these vaccines at all, according to a report from the Brookings Institute. Provision of vaccines to the uninsured, who are at increased risk of Covid, will almost certainly deteriorate when neither administration nor the products themselves are publicly funded. And co-pays and deductibles for treatments like Paxlovid will presumably pop up for the privately insured.
The partial decommercialization of the financing of Covid care was a departure from business as usual for American health care. Many were struck by the novelty of walking into a mass vaccination site and being able to get a vaccine free of charge without an insurance card, or of being able to order free Covid-19 tests online from the government. As a pulmonary physician, I’m more confident that the sorts of patients I see with advanced lung disease will be able to get Paxlovid or a Covid vaccine than, say, an expensive inhaler for asthma. So it is unfortunate, if unsurprising, to watch Covid become yet another illness inadequately covered by a faulty and fragmented financing system.
We will experience Covid waves for the foreseeable future, probably indefinitely, which means that it will remain a public health threat for some time: It was, that is to say, inevitable that financing care for this illness would ultimately be incorporated into the fabric of the American health care system. But rather than shift the way we finance Covid care so that it resembles everything else in American medicine, we should do the opposite: realize a universal, integrated, primary care–based national health program that more efficiently provides the full spectrum of health care—including prevention and treatment of Covid-19—on the basis of needs, not means.