The sudden overdose deaths of Philip Seymour Hoffman and Prince, in 2014 and 2016, happened during wall-to-wall coverage of an emerging crisis, which had come to be known as the “opioid epidemic.” A 60 Minutes investigation in 2015 titled “Heroin in the Heartland” was premised on heroin’s changing profile. “The faces of heroin include the young, middle-to-upper class and suburban,” the synopsis reads. “What was once thought of as an inner-city problem is now a national epidemic.”
Major media outlets each did their
own version of the “new face of heroin.” That new face was young, white, and “all-American.” In the 2000s, many cases of addiction to heroin began with pharmaceutical opioids that
had flooded the market since the late 1990s, thanks in large part to toothless regulators captured by corporate interests. A glut of high-dose
opioids like oxycodone
flowing through the medical market found a young,
white consumer base in the illicit market willing to pay top dollar. But things took a dark turn around 2010, when pharmaceutical opioids became scarce, expensive, and tamper-proof,
which sparked a mass exodus from pills to cheap, potent, and widely available heroin. Some experts thought a “rush” to the heroin market wouldn’t be all that bad, but since the crackdown on pharmaceutical opioids,
overdose deaths continue to break annual records. Thousands died because they were now using drugs in an unregulated, criminalized environment.
But because pharmaceutical opioids were pinned as the gateway to heroin addiction—even though many heroin users were never prescribed opioids themselves—the media did not demonize these new users as “junkies.” This “new face” narrative also posited that drugs like heroin were leaving “urban” centers and invading America’s idealized heartland, places like the Ohio River Valley and Appalachia, where drug use and addiction do not belong (aside from alcohol, of course).
“The crux of the typical media story on OxyContin was the defilement of white innocence: suburban cheerleader to sex worker, rural honors student to criminal,” writes historian David Herzberg, author of a new book, White Market Drugs: Big Pharma and the Hidden History of Addiction in America. A historian of medicine and the pharmaceutical industry, Herzberg saw the media characterize rising addiction and overdose deaths as something unprecedented—new faces, new places, new drugs. Having just written Happy Pills in America, tracing the rise of blockbuster pharmaceuticals like Prozac and Valium, Herzberg knew there was something off about the “new face” story. “To see the opioid crisis as new and unprecedented in this way required a radical act of forgetting,” Herzberg writes.
What have so many of us forgotten? In the style of a classic work of alternative history, Herzberg’s White Markets reminds us that over the last 150 years, pharmaceutical boom and bust cycles have continually hit small towns and communities across America. First, the nineteenth and early twentieth centuries saw a rise in legal opioid and cocaine sales: Think of those vintage ads for cocaine toothache drops. Next, from roughly 1930 to 1970, was a pharmaceutical bonanza of uppers and downers, from stimulants prescribed as diet pills to sedatives like quaaludes (“Disco-biscuits”) and benzodiazepines (Valium). Last, at the turn of the twenty-first century, after decades of anti-regulatory fervor promising to unleash the power of free enterprise, came a toxic mix of all past drug crises—uppers, downers, and opioids—rolled into one ongoing tragedy of record-breaking overdose deaths.
Americans, especially affluent, white Americans, have always used drugs accessed through what Herzberg calls “white markets,” legally sanctioned and trusted medical institutions like hospitals, doctors, and pharmacies. The majority of morphine users in the late nineteenth and early twentieth centuries were well-to-do white women, some of whom were maintained on morphine for years thanks to doctors who recognized that without it, their lives would be miserable. The same goes for anti-anxiety sedatives like benzodiazepines, immortalized in the 1965 Rolling Stones song “Mother’s Little Helper”:
“Kids are different today,” I hear every mother say
Mother needs something today to calm her down
And though she’s not really ill, there’s a little yellow pill
She goes running for the shelter of her mother’s little helper
And it helps her on her way, gets her through her busy day.
Herzberg asked how it’s possible to continually rediscover the fact of white
drug use as something new and transgressive. Why haven’t these
pharmaceutically driven events of the past registered as “drug epidemics” in
the way heroin does today or crack cocaine did in the ’90s? And what are the
political implications of “this bizarre, long-running national surprise?”
Part of the answer is that pharmaceuticals aren’t seen as drugs—they’re medicine. “Medicine” is legal, prescribed by a doctor, and taken for legitimate reasons, like treating pain and relieving suffering. “Drugs” are perceived to be dangerous compounds with no therapeutic value, sold to “dope fiends” on the street chasing a high. The suburban homemaker taking Valium to stay on top of things does not generate the same ire, or punitive impulse, as a Black woman like Billie Holiday using heroin. Federal authorities loathed Holiday’s song about lynching, “Strange Fruit,” and her heroin use became a pretext for constant harassment by drug warriors.
Herzberg calls this the “drug-medicine divide,” and he argues that this binary is a fatal flaw at the heart of America’s system of drug regulation and control. Like other policy inventions of the Progressive Era, the drug-medicine divide is a form of segregation—with largely white and wealthy people on one side treated as patients and consumers, and largely poorer people and people of color, on the other, treated as criminals.
The way this line is formed has less to do with scientific rationale or objective health risk than with the inescapable politics of race, class, and gender. What matters more than the properties of the drug itself is who is using it. “Many drugs, and many types of drug use, have been dragged back and forth across the line,” Herzberg writes. Opiates are a prime example. In 1877, The New York Times wrote that “morphine habitués” were an educated, high-class, and intellectually evolved crowd. “Far from being a vice,” the Times went on, using morphine “is actually a disease, produced not through the culpability of its victims, but in consequence of their physical and mental ailments, and chiefly through the instrumentality of their physicians.” Those who became regular users of morphine were “pitiable” victims of greedy or unscrupulous doctors. Harper’s Magazine also emphasized the innocence of the “vast majority of Anglo-Saxon opium-eaters” who are seduced by morphine not through any moral weakness or defect of character, but “through a medical prescription.”
A physician writing in the prestigious Journal of the American Medical Association also felt pity for those who succumbed to morphine “for relief of the pains of existence.” These morphine users were not criminals of the underworld, or even considered “addicts,” but “those who dwell among us: our fathers, mothers, brothers, sisters and friends.” That’s because addiction was a category of drug use designed for racial minorities and depraved “dope fiends.” Early twentieth-century experts had built a highly stigmatized concept of addiction by studying consumers in informal urban markets, Herzberg writes, noting that their symptoms were shaped by poverty and “anti-vice policing” more than by the substance they were using. These white morphine users showed no signs of criminality or immoral behavior, so long as they had a stable supply of morphine, of course.
At the same time that morphine use was on an upswing in the late nineteenth century, so were anti-immigrant sentiments among American nativists. White Americans feared that cheap, exploitable Chinese labor was threatening their economic prospects, which led cities like San Francisco and Chicago to pass the first laws banning “opium dens” in ghettos known as “vice districts.” That’s why, in the same article about innocent morphine users, the caring physician had this to say about those who procure opium in dens outside of tony white markets: They are “wholly given over to evil ways and the sooner they end their days the better for themselves and mankind at large.”
Sympathy for morphine users, death to opium users. The absurd fact is that morphine is not only a derivative of opium, but it’s also much more potent, especially when injected, whereas opium is smoked. Both morphine and opium are in the same class of drug known as opiates; they work by attaching to certain receptors in the brain that dull signals transmitting pain. Opiates can also produce a warm, comforting euphoria. Are the white people using morphine to treat the “pains of existence” really all that different from Chinese migrants enjoying opium after a long day of back-breaking labor in a foreign country? The drug-medicine divide separates and segregates them.
The drug-medicine binary persists today, exacerbated by inequities in the health care system. One constant throughout the history of American drug use is that racial minorities do not get to enjoy access to medicine in white markets, and therefore their drug use is always already criminalized. Even Black people who deal with painful chronic health conditions like sickle cell anemia receive inadequate pain management out of prejudice. The medical system leaves them to suffer in agony rather than prescribe relief through opioids. Herzberg notes that physicians were even once taught that Black people experience pain less intensely than whites and therefore didn’t need opioids. While the media focuses on the “new face” of the so-called heroin epidemic, the steepest death rates are actually found in older Black communities, in cities like Chicago and Baltimore, and in The Bronx, where heroin use is considered endemic and the heroin supply is contaminated with superpotent synthetic opioids. Today, Black people are 2.5 times more likely to die from an overdose than white people.
There are small glimpses of hope in the history of pharmaceutical regulation. In the 1970s, for example, rather than outright banning sedatives and stimulants, regulators aggressively stepped in to rein in pharmaceutical power and build consumer protections. Amphetamines could no longer be prescribed for weight loss (though it still happens), and sedatives were to be used on a short-term basis (though some still take them long-term). As prescriptions for speed and downers plummeted, overdoses fell, too. “Drug controls were designed not to punish consumers into abstaining from drug use but to limit the way the pursuit of profit magnified the harms of already dangerous drugs,” Herzberg writes.
Unlike cocaine, heroin, cannabis, and opium, many of the sedatives and stimulants from this era did not succumb to the iron fist of prohibition. Instead, these drugs remain accessible through a doctor’s prescription. While far from perfect, cautious regulation is a far more rational response than total prohibition. Of course, white, wealthy people still have an easier time coming by Adderall and Xanax than the average consumer, especially compared to people of color and those with a history of addiction. Those who are uninsured or under-insured cannot afford to pay for doctor’s appointments and prescriptions for these substances, either, and are thus economically excluded from white markets. But Herzberg’s point is that these policies designed to control pharmaceuticals, rather than prohibit them outright, can also be applied to the so-called dangerous substances we refer to as “drugs.” (Even writing this review is a linguistic minefield, almost impossible to accomplish without subtly reinforcing the logic of the drug-medicine divide.)
In Switzerland, for example, people addicted to heroin are able to access a legal, pharmaceutical supply of heroin that they take in sterile, monitored settings. No one dies from overdoses in these clinics, and people get their lives back because they no longer have to hustle to get the drug they need. Instead of punishing people who become addicted, a system can be designed to protect people from the dangers of the illicit market and from corporate greed, while still providing access to what they need. In the U.S. and Canada, there are grassroots movements calling for a “safe supply,” a similar setup to the one in the late nineteenth century, when physicians maintained their well-to-do patients on morphine even though it was legally forbidden.
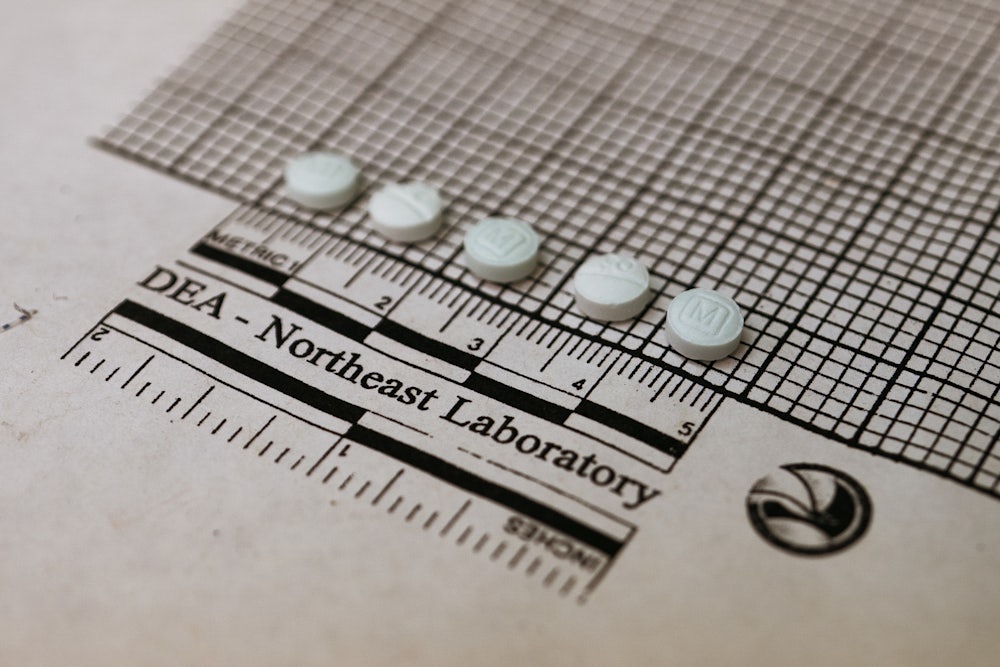
Too often in the United States, people seeking relief—or, God forbid, pleasure—have few ways to access a legal, regulated supply of substances. So they are instead forced to navigate illicit, unregulated, heavily criminalized markets. Not even rich and famous celebrities like Philip Seymour Hoffman or Prince felt they could get what they needed from white markets. What if Hoffman could have walked into a clinic and safely injected heroin? As for Prince, he suffered from chronic pain and was prescribed opioids after a 2010 hip surgery; like others who run out of legal opioids, he sought relief in the illicit market, where he purchased what he thought was Vicodin, a prescription pain reliever whose effects and dosing were no mystery to him. But the Vicodin he purchased illegally was counterfeit and instead contained illicit fentanyl that was pressed into the shape of a familiar pill to trick consumers.
American drug laws and policy are trapped in the worst of both worlds of the drug-medicine divide. Drug users die trying to navigate a criminalized and increasingly toxic drug supply. Harm-reduction strategies that make drug use safer are severely underfunded or outlawed. Federal dollars still cannot go directly toward purchasing sterile syringes for syringe service programs, even though states like West Virginia are in the midst of a full-on HIV outbreak. People using illicit drugs are still more likely to end up incarcerated than receive effective, compassionate treatment. On the medicine side, anti-regulatory, free-enterprise ideology dominates the commercial market. Look no further than today’s extensive opioid litigation, where companies shell out billions of dollars to the government while trying to maintain their innocence and, more importantly, their market dominance. Meanwhile, people in pain who do benefit from opioids are now increasingly unable to receive the care they need; pain patients with histories of taking high-dose opioids have been abandoned by their doctors, who fear heightened surveillance of their prescription activity.
To disentangle the knotty mess of contemporary American drug policy, Herzberg’s history ultimately calls to desegregate drug use. Without equitable reform, loosely regulated white markets dominated by corporate profit will keep producing generational waves of crisis, and prohibited illicit markets will continue to destroy and criminalize marginalized communities. If the history of psychoactive drugs tells us anything, it’s that humans use drugs to feel pleasure, relieve pain, and connect more deeply to themselves and others. This fact of human life does not need to cause so much destruction.