Maxanne McCormick had every reason to believe she was dying of the same degenerative dementia that killed her mother. She’d been diagnosed in 2011, when she was just in her fifties: a devastating explanation for more than a decade of migraines, pain, brain fog, and fatigue so crushing that she had to quit her job as a physician’s assistant. Once, in the early days of her illness, she’d just arrived at work at a pediatric practice in Littleton, Colorado, and was struggling to clip on her badge—a dumb, mindless task she’d done a million times—when her arm froze, then started thrashing.
After her diagnosis, she enrolled in a study at the University of California at San Francisco that was gathering some of the most extensive data ever compiled on her condition. Her biannual treks west allowed clinical researchers to measure her decline. With each trip, her health worsened. She lost the ability to walk, then to speak. Eventually, needing round-the-clock care, Maxanne moved out of the home she shared with her husband and into a nursing home, where she was the youngest resident by decades. “I was basically waiting to die,” she recalled. She read a book called Final Exit to help weigh the merits of medically assisted suicide.
In early 2016, she took yet another trip to UCSF. It began like any other, with aides escorting Maxanne in a wheelchair through the Denver airport and all the way to the research hospital, where researchers ran days of tests as they always had. But this time, when they gathered the team for a debrief, they shared an unexpected finding: They no longer believed she had degenerative dementia. Her MRIs were looking too stable for that. Instead, she had something called functional neurological disorder, or FND: a problem with brain processing that can result in significant suffering throughout the body without corresponding tissue damage. So-called functional symptoms are highly correlated with psychosocial distress and can be excruciating, despite evading most lab tests. Conceding that we lack the vocabulary to understand how the brain interacts with the rest of the body, most FND researchers reach for metaphor: FND is a software problem, not a hardware problem. It’s not the machinery itself that’s on the fritz, but the system that’s running it.
Maxanne told me all about FND early one morning over Zoom, her brown bob nearly washed out by sunlight pouring in through her home office window. After years of struggling to come to terms with her failing hardware, she said, she was determined to do whatever she could to reboot her software. She threw herself into the rehab exercises she was cautiously told might help retrain her brain: She focused on her reflection in the mirror, trying to direct the image to complete tasks she’d long since failed to will her own limbs to do. Maxanne’s tone—she is “Max” to her friends, blog readers, and journalists—gradually changed from deliberate and clinical to giddy as she recounted this part of the story. “The initial recovery was nothing short of miraculous,” she told me. Her speech returned right away. Within a week, she was walking again—first around the house, then around the block, then down the aisle at her youngest daughter’s wedding. “Of course, it was still difficult being around a lot of people and noise and things like that,” she said. Even today, things aren’t perfect. Her tremors escalate when she’s stressed, for example, and she schedules appointments in the morning to preempt afternoon fatigue. She demonstrated how her body still plays tricks on her: She could touch her nose easily when focused on my face on her screen, but got shaky when she paid attention to her own arm.

Still, Maxanne couldn’t remember the last time she felt this good, when she had so recently been certain she’d never feel good again. She read all she could about FND, aghast that she’d heard so little about it even as a health care professional. And she had an irresistible urge to share what she’d learned with all those languishing with symptoms similar to hers. She started blogging about her recovery, and soon became one of the most prominent public-facing people living with FND. “This has become sort of my life’s mission,” she told me. “I care very much about helping people who are stuck on this darn pathway.”
But not everyone is happy about her work—including many of the people Maxanne had most hoped to reach, whose illnesses bear a striking resemblance to her own. Advocates of the so-called contested illnesses that number among the most controversial topics in medicine—including chronic fatigue syndrome, or ME/CFS; chronic Lyme disease; and, more recently, long Covid—fiercely reject FND as tantamount to telling patients that their suffering is all in their heads. ME/CFS activist and documentary filmmaker Jennifer Brea insists that FND is “not a diagnosis that is ready for prime time.” Other advocates quip that it’s an acronym for “fictional non-diagnosis.” They say that their illnesses are strictly physical; the idea that their mental health could have anything to do with their symptoms is as offensive as dismissing HIV as anxiety.
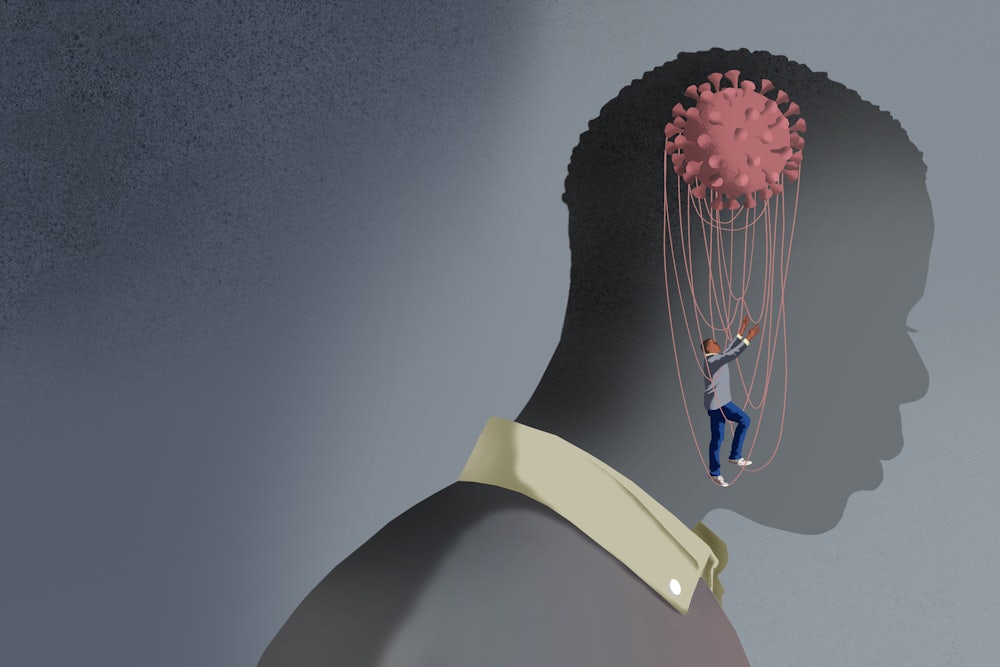
These debates have been supercharged by the rise of long Covid, a patient-coined term invoking post-viral chronic illness that lingers after sufferers have ostensibly recovered from SARS-CoV-2. Newly minted long Covid activists have teamed up with champions of ME/CFS and related diagnoses, demanding research into biopharmaceutical interventions over psychosocial research and support. The conflict reveals stark tensions between the biomedical and biopsychosocial models of medicine that get at fundamental questions of what illness is, and what medicine can and can’t do.
Symptoms like those Maxanne had—extreme fatigue, pain, involuntary tremors and spasms, dizziness, brain fog, and general malaise—have persisted throughout history, and medicine has never quite known what to do with them.
Because illness is in large part socially defined, understandings of specific diagnoses have been fluid across time and space. But the most direct precursor to FND is something you’ve probably heard of: hysteria. For most people, “hysteria” evokes an abhorrent historical relic: Hippocrates’s version of “Women are crazy.” But if the diagnosis of hysteria has undeniably misogynist roots—ancient Greeks were convinced that wombs migrated throughout the body and caused all sorts of symptoms, and clinicians retained the Greek root word hystera for “uterus” when devising an amalgamated disease centuries later—hysteria as a cohesive medical category was also considered a real and miserable malady that ravaged women disproportionately but befell men as well.
In the late nineteenth century, Jean-Martin Charcot, the so-called father of neurology, became intensely interested in hysteria. While cases shared symptoms in common with other conditions he’d described, like multiple sclerosis and Parkinson’s, the latter patients had telltale brain lesions that corresponded in key ways to their symptoms, where hysterics did not.
But soon, work on hysteria by a student of Charcot eclipsed his own. Sigmund Freud concluded that the long-observed correlation between trauma and hysteria was a straightforwardly causal link with an equally straightforward solution. In a nutshell, hysteria was the subconscious conversion of painful repressed memories, often of a sexual nature, into physical symptoms—and patients could resolve their illnesses, Freud insisted, through memory recovery and psychoanalysis. (When those methods failed, Freud had all sorts of convoluted explanations why.)
Freud’s influence helped split neurology and psychology into distinct fields, dooming hysteria to float uncomfortably between them. And in 1964, the diagnosis was dealt a major public blow that warded off clinical interest. A British psychiatrist, Eliot Slater, examined the medical records of dozens of hysteria patients who had come through his hospital and found alternate diagnoses for each. In a now famous medical lecture, he excoriated the construct altogether: “The only thing that hysterical patients can be shown to have in common is that they are all patients…. The diagnosis of ‘hysteria’ is a disguise for ignorance and a fertile source of clinical error. It is in fact not only a delusion but a snare.”
Slater’s landmark conclusions are still lauded by those convinced that hysteria was little more than a dismissive label slapped on women sick with physical ailments. These critics offer an alternative narrative: Around the same time that Charcot was searching brains for missing lesions, reports began surfacing of patients left with lingering symptoms long after an 1889 outbreak of Russian flu. A similar pattern followed the 1918 Spanish flu. In the next decades, stories of outbreaks leaving clusters of sufferers in bed reportedly sprang up dozens of times, including in a Wisconsin convent, at an Athens midwifery institute, and among nurses at a London hospital. In 1984, in the well-to-do skiing town of Incline Village, Nevada, on Lake Tahoe, more than 100 relatively young, previously healthy patients were felled by all-encompassing fatigue. But however undeniably ill they were, clinicians struggled to pinpoint objective signs suggesting any convincing single cause.
It was the famous Lake Tahoe cluster that the Centers for Disease Control and Prevention first dubbed chronic fatigue syndrome, now more commonly known as ME/CFS (which is a compromise between the original name and “myalgic encephalomyelitis,” a term preferred by patients who argue that “chronic fatigue” doesn’t capture their condition’s severity). In the face of decades of stigma—comedian Ricky Gervais infamously mocked ME/CFS in 2007 as “the one where ‘don’t feel like going to work today’”—advocates and a committed core of researchers nonetheless forged a body of knowledge about a disease that they estimate receives the lowest funding, relative to its burden, from the National Institutes of Health. One survey showed that more than 70 percent of patient respondents reported an infection had triggered their illness, and the diagnosis includes symptoms such as extreme fatigue, sleep troubles, and pain. Its defining diagnostic criterion is post-exertional malaise, or a significant depletion of energy following physical or mental exertion. For the past few years, the CDC website has offered a disclaimer in its coverage of ME/CFS: “ME/CFS is a biological illness, not a psychologic disorder. Patients with ME/CFS are neither malingering nor seeking secondary gain. These patients have multiple pathophysiological changes that affect multiple systems.”
The CDC statement was almost certainly intended as a rebuke of people like Michael Sharpe. Back in the 1980s, when the professor emeritus of psychological medicine at Oxford was still a junior researcher, an infectious-disease colleague had grown flummoxed by patients with unexplained exhaustion and pain. Sharpe spent months in that clinic, meeting with and listening to the patients, taking full histories, and reviewing the standard lab tests they’d received. And while he couldn’t say for certain why they were still so sick, he did notice that the ones suffering the most tended to be intensely focused on their symptoms, distressed about not getting better, and very worried about doing anything to make their ailments worse. Some were so anguished that it overwhelmed them. They even avoided things they’d once enjoyed. “That’s how I got involved,” he told me. “I’ve always been interested in seeing if we can do things for these patients that medicine can’t. You know, is there any way you can come from another angle here? In this case, some kind of behavioral angle that’s different than just doing lots of blood tests?” When cognitive behavioral therapy seemed to be helping people with other conditions, Sharpe wondered whether it might also help patients whose symptoms, however severe, simply didn’t line up with pathophysiological rules. In one essay, he characterized this as having “illness without disease.”
As it turned out, there were quite a lot of these patients, and Sharpe passed on his passion for treating them to his young neurologist advisees, Jon Stone and Alan Carson. In the 1990s and early 2000s, it was becoming clear that illnesses previously known as hysteria hadn’t simply vanished, sorted into more appropriate diagnostic categories, as Eliot Slater had urged decades earlier. Stone and Carson began to study the symptoms with a neurological lens, conceiving of them as misfiring brain signals rather than a Freudian cry for help. Rebranding hysteria as FND was to reject the notion that the best way to understand functional paralysis was as a subconscious repression of childhood memories. Rather, it was an interruption in the brain processing that facilitates the executive function of your legs—a blip that could be triggered by all sorts of things.
In other words, stress could exacerbate FND, and someone with FND could overfocus on symptoms and essentially turn up their volume, requiring brain processing for actions that should be automatic. As Carson put it to me, the term “functional neurological disorder” should be reserved for neurological symptoms like weakness, seizures, memory loss, or cognitive issues. “Functional symptoms” and “functional disorders” are largely used interchangeably about other parts of the body. Irritable bowel syndrome, for example, is widely theorized to be a functional disorder. Meanwhile, conditions like depression and anxiety frequently include symptoms most people would describe as physical. It’s even possible to have functional and nonfunctional symptoms at the same time. “We wonder why people get confused!” Carson quipped.
If defining these concepts can be tricky for the experts who spend most of their time on them, imagine how much gets past other clinicians. Some 20 years ago, Dr. Mark Hallett was gobsmacked by just how badly medicine was handling these cases. As a chief investigator at the National Institute of Neurological Disorders and Stroke at the NIH, he’s invited referrals from clinicians across the country for decades of tough-to-diagnose patients presumed to have rare neurological diseases. “I began to get the sense that we were seeing large numbers of what we were calling ‘psychogenic disorders’ at the time,” Hallett told me. “Around 30 percent of our cases had a functional diagnosis. And I said, ‘Gee, this is a major problem.’” In 2006, Hallett went so far as to describe as a crisis medicine’s inability to grasp such common manifestations of illness.
“I began to look into the current landscape, and it turned out there was very little that was understood about functional disorders at all,” he told me. “Very little in textbooks, very little teaching. There was virtually no research going on. No one had much interest.”
In 2020, that changed for good.
In the early days of the Covid-19 pandemic, the contours of a by now familiar story began to reveal themselves. After being infected with the novel coronavirus, some people weren’t recovering as quickly as expected. In mid-April 2020, journalist Fiona Lowenstein published an op-ed in The New York Times called “WE NEED TO TALK ABOUT WHAT CORONAVIRUS RECOVERIES LOOK LIKE.” Lowenstein had founded a survivor support group for people whose symptoms still hadn’t resolved after many weeks. Soon, an infectious-disease specialist at the Liverpool School of Tropical Medicine, Paul Garner, wrote a series of blog posts for the British Medical Journal about the harrowing aftermath of his Covid-19 illness: “For 7 weeks I have been through a roller coaster of ill health, extreme emotions, and utter exhaustion,” one headline read. In subsequent posts, he described intense brain fog, tinnitus, and a bad relapse after hitting an aerobics class: “I was more exhausted than ever and could not get out of bed for three days,” he wrote, a spot-on description of “post-exertional malaise,” although he didn’t know that at the time. In June 2020, Lowenstein and Garner were both key sources in Pulitzer Prize winner Ed Yong’s first Atlantic feature about what patients in online support groups soon dubbed “long Covid.”
More stories from Yong and many others followed, and the picture they painted was frightening. People who had relatively mild initial bouts of Covid-19 were in awful shape weeks, months, and even a year or more later. One early feature described sufferers experiencing “extreme fatigue, bulging veins, excessive bruising, an erratic heartbeat, short-term memory loss, gynecological problems, sensitivity to light and sounds, and brain fog.” Others developed new allergies and extreme itchiness, bouts of blindness and paralysis, or joint pain and hair loss. Plenty of patients were falling ill after apparently asymptomatic cases of Covid-19. After the slow-to-recover started gathering online, one survey identified 200 symptoms associated with the emerging malady.
Almost immediately, ME/CFS advocates recognized what was going on: Long Covid, they believed, was simply the latest wave of their own disease, which often followed viral infection. Thanks to the sheer scale of the coronavirus pandemic, its existence was more undeniable than ever. As Jaime Seltzer of the advocacy group MEAction put it to WebMD, if the portion of people who end up with long-lasting illness is “similar to what has been seen for other pathogens, then we’re looking at a mass disabling event.” Subsequent studies have suggested that around half of people with persistent symptoms after Covid-19 fit the diagnostic criteria of ME/CFS. Seeing common cause, existing advocacy networks allied with newly minted long Covid advocates. MEAction has reportedly contacted hundreds of journalists and clinicians since the start of the pandemic to emphasize the connection between ME/CFS and long Covid.
Almost three years into the SARS-CoV-2 pandemic, their arguments have become the consensus of experts around the world, shaping public and professional understandings of long Covid as a complex, chronic, organic disease neglected by science. Meanwhile, so much research piled up suggesting physiological dysfunction linked to long Covid that some people began to wonder if the overall toll of long Covid exceeded that of the acute disease. Studies have linked long Covid to immune dysfunction, chronic inflammation, tiny blood clots that depleted the brain of oxygen, and even the Epstein-Barr virus, which strong evidence suggests may cause multiple sclerosis.
Most recently, a study led by Yale immunologist Akiko Iwasaki and Mount Sinai physical therapist David Putrino offered further evidence of measurable physiological abnormalities in long Covid patients: reduced T cells, for example, and lower levels of cortisol. “We hope our study will be informative to others working in the field,” Iwasaki reflected on Twitter upon the release of the preprint. “We also hope that these data will help those who are still skeptical understand that long COVID is real, and it has a biological basis.”
But Long Covid was never exactly as cut and dried as some quarters made it out to be. If advocates have seen the past few years as an overdue reckoning for medicine’s eternal indifference toward women and the diseases that disproportionately befall them, others have seen it as something else: a dramatic illustration of suffering driven by psychosocial distress, and how poorly medicine is equipped to handle it.
The latter case goes something like this: A chronic illness that appeared to be triggered by viral infection could just as easily have been triggered by the trauma of the pandemic itself. That long Covid, ME/CFS, and related diagnoses disproportionately target women perhaps stems from the fact that, in a patriarchal world, women face more adversity and have less control over their lives.
The eye-popping range of issues linked to long Covid raises questions about whether all are ascribable to viral infection, particularly since two of the most widely reported symptoms—fatigue and brain fog—are also commonly associated with stress, depression, anxiety, and functional disorders like FND. Since 2019, rates of people reportedly experiencing depression and anxiety have quadrupled, according to some estimates; loneliness and isolation spiked as well. One recent study found all of these things to be highly correlated with long Covid. Cell-level and hormonal findings along the lines of those in the Putrino and Iwasaki study have also been observed in chronic pain, post-traumatic stress disorder, and depression, but often don’t seem to correlate with symptoms, and it’s unclear what any of it means clinically, or whether there’s any causal relationship. Finally, an NIH-sponsored longitudinal study on long Covid—the most thorough and detailed analysis of the condition yet produced—found no tissue damage in long Covid patients, no evidence of viral persistence, and no abnormalities in any organ function relative to controls. “We are finding little to no abnormalities,” lead author Dr. Michael Sneller told NPR before the study’s publication. “Echocardiogram, pulmonary function tests, X-rays, brain MRIs. You name it. Laboratory markers of organ dysfunction. We’re not seeing any of that … and precious little evidence of immune activation.… I’m running out of tests to do, basically.” One association his final paper did find, however, was an association between long Covid and anxiety disorder.
Furthermore, the association between infection and acute illness with long Covid appears tenuous. A detailed early cohort study conducted by patients themselves found that, while the availability of PCR testing lagged early in the pandemic, the majority of participants eventually underwent antibody testing—but over two-thirds of those participants tested negative, suggesting that even after accounting for false negatives, and for the possibility of antibodies never materializing or fading over time, at least some portion of them never had Covid-19 to begin with. Other long Covid research raises questions, too: Some widely cited studies used no control groups, made inappropriate comparisons (for example, contrasting debilitated long Covid patients with self-reportedly healthy people instead of, say, people with extreme depression), or were published in borderline predatory pay-to-play journals with dodgy peer review processes.
Meanwhile, there is evidence hinting that some symptoms chalked up to long Covid may well be functional. Alan Carson, one of the leading neuropsychiatrists on functional symptoms, told me that he’s seen plenty of FND and other functional disorders at long Covid clinics in Edinburgh. Many studies are missing detailed clinical assessments by experienced physicians, he told me, relying instead on brief sessions with intake nurses and searches for novel biomarkers. In one case, he reexamined long Covid patients who had undergone much shorter evaluations in a previous study, and found context other investigators had missed. He determined that one long Covid patient who was unable to walk had functional paralysis that was likely triggered by his traumatic hospitalization early in the pandemic: “He’d been awake and conscious much of the time he’d spent in the ICU,” Carson told me. “And he’d been exposed to a lot of people dying in pretty horrible ways, thinking, ‘Oh, I’m next.’” For Carson, the idea that the etiology of this man’s symptoms would render him less worthy of care or sympathy than someone whose symptoms are caused by physical tissue damage is troubling. Some people are willing to “feel sorry for the sufferers,” he said, only “if we find a traditional pathogenic mechanism … and that, to me, seems a fundamentally flawed point.”
Mark Hallett, the NIH doctor, has also seen functional symptoms within both long Covid and ME/CFS cohorts. “Some patients will have an organic etiology for their post-Covid syndrome, other patients will have a functional etiology,” he told me. “We don’t want to say that any diagnosis is bad. Functional disorder is not voluntary. People are not doing it to themselves. That’s just the way the brain is reacting to their particular situation.”
Does that mean that long Covid is “all in their head”? In one way, no—of course it doesn’t. The symptoms are real, and patients’ testimony about them is sacrosanct. They are not confused, faking, or unreliable. They’re sick. But in another way, the head encases the only organ capable of experiencing any illness at all—and whose function is irrevocably affected by love, poverty, angst, violence, terror, geography, housing, monotony, hopelessness, and so on and so on. There’s no feeling or interpreting anything outside of your brain. So yes, perhaps long Covid is all in your head. Just like everything else.
For all their disagreements, proponents of the biomedical and biopsychosocial models of long Covid share considerable common ground. The Covid-19 pandemic has driven widespread debility, whether a result of distress or the virus itself, compounded in either case by political abandonment and public health failures. Both camps emphasize that patients are really suffering, and that it isn’t their fault. Where they diverge is on questions of treatment.
By the mid-2000s, Michael Sharpe had spent years treating the kinds of patients he’d first come across at the infectious-disease clinic at Oxford: people with persistent, chronic symptoms that were sapping the brightness from their lives. He couldn’t make patients’ lives perfect, but he could help them improve. “It’s basically just what we used to call rehabilitation,” he told me. “It’s helping people accept the situation they’re in, to give them some hope for the future and help them gradually move forward.”
In 2005, Sharpe began recruiting patients to participate in the largest-scale clinical trial ever run on ME/CFS to see if his restorative methods could help those patients, too. The PACE trial study protocol, which was designed in collaboration with a British ME/CFS patient charity, strove to determine whether graded exercise therapy, or GET, and cognitive behavioral therapy could improve outcomes. In 2011, Sharpe and his co-authors published their answer: GET and CBT did moderately improve the health of ME/CFS patients. Few study participants made a miraculous turnaround, and some didn’t respond much at all, but there was an undeniable if modest boost overall. That made GET and CBT the only clinically validated treatment for ME/CFS.
Four years later, journalist David Tuller wrote a 15,000-word critique of the PACE trial, which he called “bogus and really terrible research.” Dozens of researchers, clinicians, and advocates joined him in his criticism. They wrote an open letter to The Lancet calling for an independent investigation, circulated a petition demanding a retraction, and condemned the trial in other outlets.* An extended court battle forced Sharpe and his co-researchers to hand over their data, which detractors reanalyzed and claimed undermined the PACE conclusions. The psychologist David Marks, editor of the Journal of Health Psychology, summarized his objections to what PACE represented: “Gaslighting has been applied to the entire ME/CFS community by misapplication and misuse of the biopsychosocial model.”
Considering PACE’s ultimately rather mundane finding, the tenacity of the response is surprising. “It’s quite hard to think of any chronic illness where some psychologically informed rehabilitation doesn’t help,” Sharpe told me. Ditto for carefully graded exercise. Today, despite the blowback, Sharpe stands by his research. “It’s been hammered probably like no trial in history ever has. It’s been debated in the U.K. House of Parliament three times. It’s still there—no one has killed it.” Neither The Lancet nor the Medical Research Council UK disavowed it. More importantly, he said, “some people’s lives will be damaged because they won’t have rehabilitation when they could have, and that’s terrible.”
What he’s saying is hardly a stretch. Advocates have successfully gotten GET and CBT withdrawn from official ME/CFS treatment guidelines in the United States and the U.K. and have also objected to it as a treatment for long Covid. The Atlantic’s Ed Yong—the most respected reporter in the world on long Covid—labeled PACE “now discredited,” and warned that anyone with post-exertional malaise who pushes themselves to exercise could get “permanently worse”—a claim that isn’t evidence-based, and that would make the condition suspiciously unique in the annals of medical knowledge. MEAction is running a PSA campaign geared toward warding viewers away from the treatments validated by PACE. Its website contains links to anecdotes about patients who say they had to go to bed or use wheelchairs after short walks.
Even worse, hucksters and fringe quacks have reportedly begun administering all sorts of unproven treatments, and affixing long Covid patients with dubious diagnoses requiring unsubstantiated tests and treatments. Some patients have been prescribed anticoagulants on the off chance they will zap “microclots” coursing through their bloodstreams, and these drugs have left them at unnecessary risk for severe bleeding. Shady proprietary companies with no peer-reviewed publications promise they can both diagnose and treat the condition. Notorious ivermectin diehards have pivoted to long Covid. Moreover, it’s likely that patient exploitation that’s been seen in ME/CFS and other contested illnesses could soon target a new chronically ill population. So-called Lyme-literate M.D.s with invariably cash-only practices have bilked patients with useless tests and baseless interventions like long-term antibiotics repeatedly shown not to work, and too frequently used for patients without proven Lyme disease. In recent years, there has been an uptick in off-label neurosurgeries for ME/CFS, one of which reportedly left a young patient in the U.K. with disastrous complications.
For Maxanne McCormick, the former physician’s assistant who recovered from the worst of FND with methods resembling CBT and GET, the risky treatments patients get sucked into are disturbing. But she understands how such sick people could feel abandoned by medicine—after all, she once felt that way, too.
When she started getting sick, before her diagnosis of degenerative dementia, she was diagnosed with “conversion disorder,” the Freudian diagnostic label that succeeded hysteria and preceded FND. Back then, even fewer clinicians understood how to handle functional symptoms, and the standard of care was basically to shrug and send the patient home, or shunt them off to therapy. Maxanne felt alienated by the diagnosis, and the doctors weren’t helpful—plenty, of course, still aren’t. “It was really horrible to go for help and be treated with contempt,” she recalled. “It just cuts at your soul. And I didn’t ever want that to happen again.” Maxanne did try therapy, and even appreciated it—it helped her begin to process an abusive childhood. But she couldn’t see how it was connected with her migraines, fatigue, or tremors.
So Maxanne shied away from further treatment, and her health gradually got worse. It was another 15 years before medicine finally began to get it right.
It’s tempting to see Maxanne’s story as yet another illustration of a point often made about long Covid: As public health professionals Steven Phillips and Michelle Williams put it in The New England Journal of Medicine last year, “Our medical system has a long history of minimizing women’s symptoms and dismissing or misdiagnosing their conditions as psychological.”
Perhaps, but the truth is more complicated than that. In a profit-driven system, if some symptoms get minimized, others are maximized. Eli Lilly, for example, famously spent years marketing the concept of extreme PMS to generate novel demand for Prozac, whose patent was about to expire. Thanks to overdiagnosis and overtreatment, 25,000 women in the United States undergo unnecessary breast cancer treatment each year, per one recent estimate. It’s widely acknowledged that most C-sections are not medically necessary. And while misdiagnosis does happen, it’s arguably worse to err on the side of biomedicalization: For example, FND patients with functional seizures have been inappropriately prescribed antiepileptic drugs with serious side effects. And it’s no coincidence that Eliot Slater, the mid-century neurologist who fiercely denounced the concept of hysteria, was also one of history’s most enthusiastic defenders of lobotomies.
It’s tiresome how often statements like “dismissing women’s conditions as psychological” go unchallenged—as if so-called psychological illnesses are frivolous or fake rather than some of the most persistent and irrevocable drivers of human suffering. After decades of biomedical research, we’re just as far from curing depression as we are long Covid: For the majority of patients, antidepressants barely beat placebos. Chronic pain, too, has stymied biomedicine: Research shows little correlation between observable anatomic abnormalities and the lived experience of pain. When suffering has no clear physiological etiology, it’s usually tougher to solve. We have little control over the social and material contexts of our lives, and couldn’t eliminate misery or illness even if we had more.
Over the last two centuries of the history of medicine, there have been a few breakthroughs that transformed how we think about our lives. Most people can recite the basic outlines of such discoveries: Some mysterious malady killed countless people, until a drug or vaccine came along that vanquished or dramatically tamed the disease—a story that’s more or less true for syphilis, yellow fever, smallpox, measles, polio, and even HIV.
For those who see contested illnesses through a biomedical lens, this history is inspiring, and the need for scientific research into cures is a no-brainer. But the model doesn’t work for every type of suffering. There is unlikely ever to be a penicillin for long Covid or ME/CFS. Indeed, even as we’ve churned out pills and shots that target specific pathogens and render the scourges of yesteryear practically irrelevant, we’ve never gotten very good at treating some of our most common chronic symptoms, such as brain fog, fatigue, and pain. Drugs can zero in on a pathogen, but they aren’t so good at targeting the biopsychosocial factors that shape our well-being.
Several years into a global pandemic, it’s appalling how often medicine struggles to identify—let alone appropriately treat—functional disorders or symptoms provoked by psychosocial distress. When faced with such patients, the most odious doctors will drop them down a chute into crankland, where they’ll be subject to a dubious or even dangerous barrage of tests, tweaks, and experimental procedures rarely billable to insurance. Many others will do what they did to Maxanne back in the early 2000s—pathologize them and send them away.
As she tells it now, Maxanne needed her illness to be socially legible. That’s why she was perversely happy to be diagnosed with degenerative dementia back in 2011: “I preferred a terminal diagnosis that gave me a feeling of dignity, and people can look at you and go, ‘Oh, I’m so sorry, I can now give you my support,’ instead of ‘That’s really weird.’”
But once she heard Jon Stone from Edinburgh explain FND, she realized her illness wasn’t so weird after all: “Your brain is not sending and receiving signals correctly from your body,” she remembered Stone explaining. “And so your body’s not functioning correctly right now. But there is hope, and you’re not making it up. We know that this is very real. But there are ways we can address those connections and reestablish the correct connections again.”
Zachary Grin, a physical therapist specializing in FND, told me that, unlike conventional rehab with a more specific focus—say, leg strengthening exercises after a leg injury—functional symptoms require more systemic work to reset the connection between brain and body. He asks patients to count backward by three during exercises, or practice going up stairs backward, to reset their autopilot. That is more or less what Max and her care team have tried to do, through rehab drills, stress management, habit building, and practicing various motions in the mirror. Paul Garner—the infectious-disease doctor in the U.K. who wrote some of the earliest first-person pieces about long Covid—recovered in a similar way. Both say that embracing a biopsychosocial framework has been key to their recovery, and they have concerns about how the dominant media narrative is affecting patients. “I had to stop the Facebook groups, get away from talking about my symptoms, and try to put them into context,” Garner told me.
People like Maxanne and Paul were fortunate to get better from the worst points in their lives. So many people don’t. What both of them had—and what every ill person deserves, regardless of the cause of their symptoms—is support. They were loved and helped by family members, able to survive without working during their illness, and enjoyed secure housing and access to good health care—all the tools they needed to thrive.
Once we finally recognize how dramatically illness is driven by psychosocial distress, we can get to work engineering less of it through politics. We can provide better social and disability support for sick people, give them time to convalesce, redistribute resources so that no one is balancing their health on the edge of their last nerve. We can fund robust childcare, family leave, and early childhood education to alleviate the systemic strain that burdens women and disproportionately makes them sick. We can fight for universal health care built on a comprehensive primary care system, so that doctors and patients develop meaningful clinical relationships over time, and patients can discuss their concerns and manage symptoms over time in appointments less encumbered by revenue maximization.
In the meantime, we can do more to educate clinicians and the public that patients like Maxanne deserved dignity and empathy all along. More and more people are starting to agree, a change Maxanne felt acutely at the FND Society conference in Boston earlier this year. “Twenty years ago, I never could have imagined so many people would be interested in helping patients with FND,” she said. “We’ve been considered problem patients, difficult patients, the time-wasters.… I think we need to get the word out that this happens to normal people, good people. It’s common: just people struggling with an illness that has been looked at in a very terrible way for many years. And those things aren’t right. It’s just a brain disorder.”
* This article originally mischaracterized an open letter to The Lancet.